














































Study with the several resources on Docsity

Earn points by helping other students or get them with a premium plan


Prepare for your exams
Study with the several resources on Docsity

Earn points to download
Earn points by helping other students or get them with a premium plan
Community
Ask the community for help and clear up your study doubts
Discover the best universities in your country according to Docsity users
Free resources
Download our free guides on studying techniques, anxiety management strategies, and thesis advice from Docsity tutors
How to cover high blood pressure quickly
Typology: Cheat Sheet
1 / 54

This page cannot be seen from the preview
Don't miss anything!













































Standard Treatment Guidelines - Hypertension Page 1
Standard Treatment Guidelines - Hypertension Page 1
Standard Treatment Guidelines - Hypertension Page 1
low cost ACE inhibitors, (low cost Angiotensin Receptor blockers in case patients develop side effects to ACE inhibitors) , and beta-blockers. Lifestyle changes are a vital component of management of hypertension, and may be sufficient for control of mild hypertension.
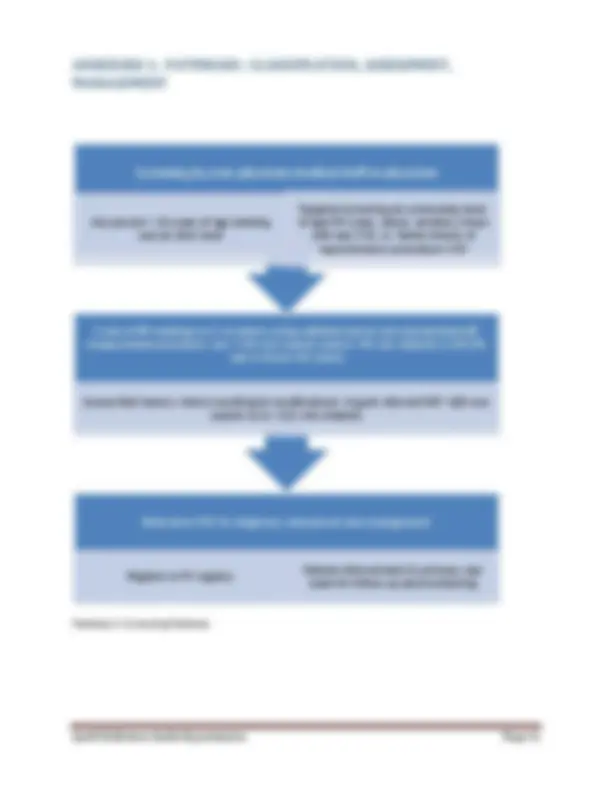
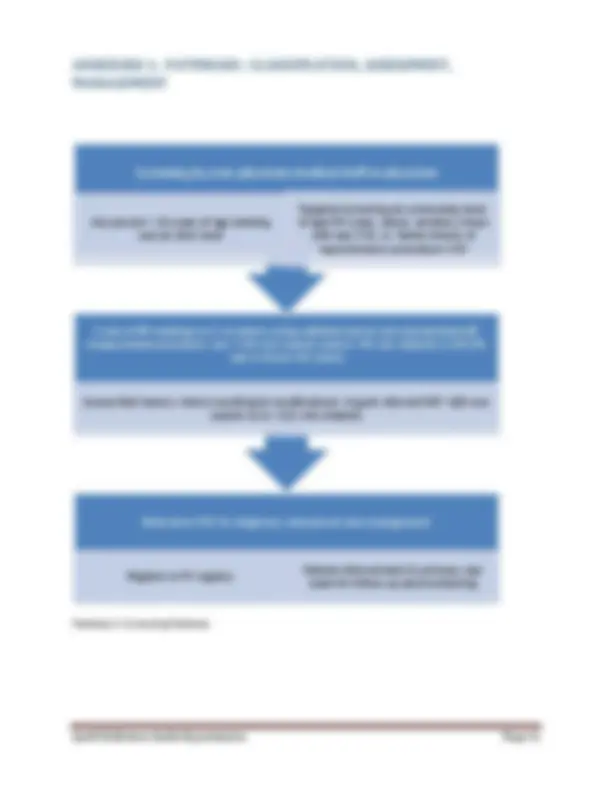
providers in the local public health system, promote adherence to therapy by simplified regimens, and monitoring by allied health staff. Figure 1 : Clinical pathway for hypertension care
1. SCREEN FOR HYPERTENSION Screen For HT (Using Opportunistic & Targeted approaches) By Physicians At All Levels Of Care and by Non-Physicians At Community Level Using A Standardized BP Measurement Procedure 2.CONFIRM DIAGNOSIS OF HYPERTENSION AND CLASSIFY HYPERTENSION Diagnosis to be confirmed by PHYSICIANS, based on at least 2 measurements taken in the clinic or by a healthcare provider on at least 2 visits, which are at least 1-4 weeks apart, (except in the case of hypertensive urgencies and hypertensive emergencies) 3.EDUCATE PATIENTS. ASSESS LIFESTYLE FACTORS, TARGET ORGAN DAMAGE, ASSOCIATED CLINICAL CONDITIONS. Establish rapport with patients. Educate them about asymptomatic nature of disease which has risk of serious complications which can be prevented by achieving and maintaining target BP by regular therapy. Emphasize importance of lifestyle modifications to lower BP and cardiovascular risk. Assess lifestyle related and other cardiovascular risk factors, target organ damage, associated clinical conditions by using a combination of history, examination and investigations. Assess overall cardiovascular risk. Suspect secondary hypertension in appropriate setting. 4.MANAGE HYPERTENSION ( LIFESTYLE MODIFICATIONS ± DRUG THERAPY) Use Lifestyle Modifications in all patients. Initiate Drug therapy with first line antihypertensives (calcium channel blockers, ACE Inhibitors (ARBs if indicated), thiazide /thiazide like diuretics in Grade 2 /3 HT and in Grade 1 HTwhen indicated. Titrate drug therapy using optimal doses of one or more classes of drugs to achieve target BPs. Manage comorbidities like diabetes and associated clinical conditions (heart disease, CVD, CKD) Manage hypertension appropriately in special groups (elderly) and special situations (urgencies and emergencies) Use other measures to reduce cardiovascular risk if indicated ( statins, aspirin ) 5.FOLLOW UP AND MAINTAIN ADHERENCE. Preferably follow up at Primary Care level with a team based approach. Review BP and advice on adherence. Reassess target organ damage, risk factor s periodically. Review and advice on adherence to life style modification. Refer in case of hypertension uncontrolled on 3 drugs, suspected secondary hypertension, and in hypertensive emergencies.
1.1 An ongoing initiative to increase awareness of hypertension as a widely prevalent but asymptomatic disease associated with many adverse outcomes like heart attacks, strokes, heart failure, kidney failure. Early diagnosis and effective control of BP can save people from much morbidity, mortality and disability. 1.2 All adults above the age of 18 years should undergo opportunistic screening by healthcare providers at all points of care in India, either during the course of their visits to the health facilities, or separately as a screening examination if requested by the person. Targeted screening at the community level of high-risk groups like adults above 50 years of age, persons with diabetes, obese, smokers, those with existing cardiovascular diseases, family history of hypertension, can be undertaken by trained non-physician staff. a physician or trained non physician staff, using an automated BP instrument or any other validated device, and following a standardized BP measurement procedure, mentioned in table 1 below. TABLE 1- STANDARDIZED BP MEASUREMENT PROCEDURE – STANDARD PROCEDURE FOR BP MEASUREMENT 1.Patient preparation and position Patient should be in a relaxed state for 5 minutes before measurement of BP. Patient should not have had caffeine in the past 1 hour or smoked in the past 30 minutes. Patient should be seated comfortably with back supported, with arm at heart level, and legs in an uncrossed position. 2.Choice of BP device Mercury sphygmomanometer or any other device (including electronic digital oscillometric devices) which has been validated using a standard protocol, and has been calibrated regularly. 3.Cuff size and placement The cuff size should be appropriate for the patient. Length of bladder should be 80% of arm circumference and width should be 40% of arm circumference, and a large adult cuff should be used for an obese patient. Patient should not wear any constrictive clothing. Place the midline of the cuff over the pulsations of the brachial artery, at a distance of 2-3 cm above the cubital fossa.
130 - 139 85 - 89 Advise lifestyle modifications: Recheck in 1 year 140 - 159 90 - 99 Recheck BP within 1-2 weeks. Advise lifestyle modifications. Refer to nearest health facility within 1 month for diagnosis, assessment. 160 - 179 100 - 109 Recheck BP within 1 week. Advise lifestyle modifications. Refer to nearest health facility for confirmation of diagnosis and initiation of treatment.
180 >110 Check for any symptoms/signs of any acute target organ damage (assess symptoms and signs referred to in the mnemonic ‘ABCDEFG’^1 mentioned in pathway on assessment and management of hypertensive crisis). In cases of acute target organ damage, treat as hypertensive emergency. Refer to PHC/CHC for evaluation and treatment immediately after confirming elevated readings in this range. Initiate therapy before referral, if seen at PHC.
2.1 Diagnosis of hypertension should be made at primary health centres and facilities above that level using validated and calibrated BP measurement devices and following the standardised BP measurement procedure. 2.2 Diagnosis of hypertension should be based on at least 2 measurements taken in the clinic or by a healthcare provider on at least 2 visits, which are at least 1-4 weeks apart, except in the case of hypertensive urgencies and hypertensive emergencies, where hypertension is diagnosed during the first visit itself.Ambulatory blood pressure monitoring and home based BP monitoring is not feasible for diagnosis for most patients with hypertension in India and is therefore not generally recommended. They may be considered where indicated e.g. in patients with suspected white coat hypertension, when the expertise and the facility is available. 2.3 Hypertension should be diagnosed when BP is persistently above a systolic of 140 mm and/or diastolic of 90 mm. 2.4. Patients with hypertension should be classified in the manner given in the table below: (^1) Abbreviation explained - A: Altered consciousness B: Breathlessness C: Chest pain(Ischemic) D: Deficit (weakness of limbs) or Decreased Urine output E: Edema F: Fundus if feasible which is showing hemorrhages, exudates, papilledema G: Generalised seizures
Category SBP(mm Hg) DBP(mm Hg) Optimal <120 and< Normal 120 – 129 and/or 80 – 84 High Normal 130 – 139 and/or 85 – 89 Grade 1 Hypertension 140 – 159 and/or 90 – 99 Grade 2 Hypertension 160 – 179 and/or 100 – 109 Grade 3 Hypertension ≥ 180 and/or ≥ 110 Isolated Systolic Hypertension ≥ 140 and < 90 Hypertensive urgency >180 and/or > Severe asymptomatic hypertension with no evidence of acute target organ damage Hypertensive emergency >180 and /or >110- 120 Severe hypertension associated with cardiovascular (e.g. left ventricular failure, cerebral (e.g. hypertensive encephalopathy, stroke),renal (acute renal failure), Grade III-IV retinopathy
b. Assessing the target organ damage related to hypertension viz. heart failure, left ventricular hypertrophy, proteinuria, retinopathy. c. Assessing the presence of associated clinical conditions like diabetes, kidney disease or symptomatic cardiovascular disease with angina, myocardial infarction, cerebrovascular disease (stroke, TIA) or peripheral arterial disease. d. Assessing the clues to a secondary cause of hypertension - see table below: Assess target organ damage : Heart (heart failure), Kidney, and Retina History Breathlessness on effort Swelling on feet Examination Raised Jugular venous pressure, edema, gallops on auscultation (heart failure) Funduscopic evidence of hypertensive retinopathy-hemorrhages, exudates, papilledema Laboratory evaluation ECG: SV1 +RV6 > 3.5 Mv (LVH) Urine protein, Serum creatinine Assess associated clinical conditions : Myocardial infarction, Stroke, Chronic Kidney disease History: Episode of chest pain at rest (Myocardial infarction) in past Weakness on one half of body (Stroke) in the past Examination: Significant pallor in the presence of HT– chronic kidney disease Laboratory: S. Creatinine ECG: Ischemia, infarction, conduction disturbances, arrhythmias (atrial fibrillation) Assess clues to presence of secondary hypertension History : Abrupt onset of hypertension below the age of 30 years and above the age of 60 years (renovascular hypertension) Paroxysms of palpitations, pain(headache), perspiration( pheochromocytoma)(^1 ) Snoring at night, breathing pauses reported by partner, daytime sleepiness (sleep apnoea) Drug intake: NSAIDs, Steroids, Oral contraceptive pill Examination : mooning of facies, striae: Cushing syndrome Unequal pulses: diminished/absent radial pulses- Takayasu’s arteritis Diminished & delayed femoral pulse in lower limb: Coarctation of aorta. Tachycardia and postural hypotension (pheochromocytoma) Bruit over renal arteries: renal artery stenosis (renovascular hypertension) Laboratory investigations : Abnormal urinalysis (proteinuria, haematuria), elevated creatinine. Abnormal kidneys on USG- renal parenchymal disease, renal artery Doppler for renal artery stenosis.
e. Assessment of overall cardiovascular risk of a patient. As seen in the table below the overall cardiovascular risk increases with the grade of HT, number of risk factors, presence of organ damage, diabetes, symptomatic cardiovascular disease or chronic kidney disease. Grade 1 HT Grade 2 HT Grade 3 HT No risk factor Low risk Moderate risk
High § risk 1 - 2 risk factor* Moderate risk Moderate to high High risk
3 risk factor* Moderate to High risk
High High risk Target Organ damage, DM, CKD stage 3 High risk High risk Very high risk Symptomatic CVD( stroke, coronary artery disease), diabetes with organ damage, CKD>stage 4 Very high risk Very high risk Very high risk
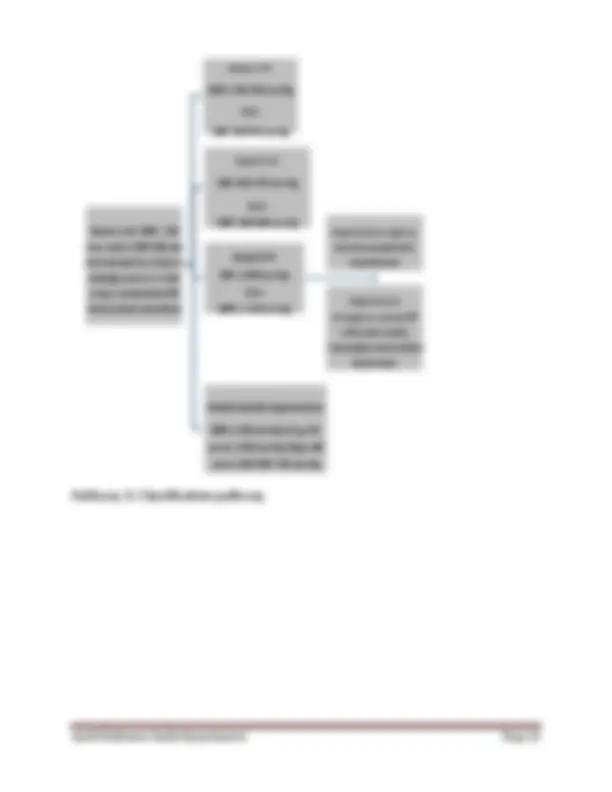
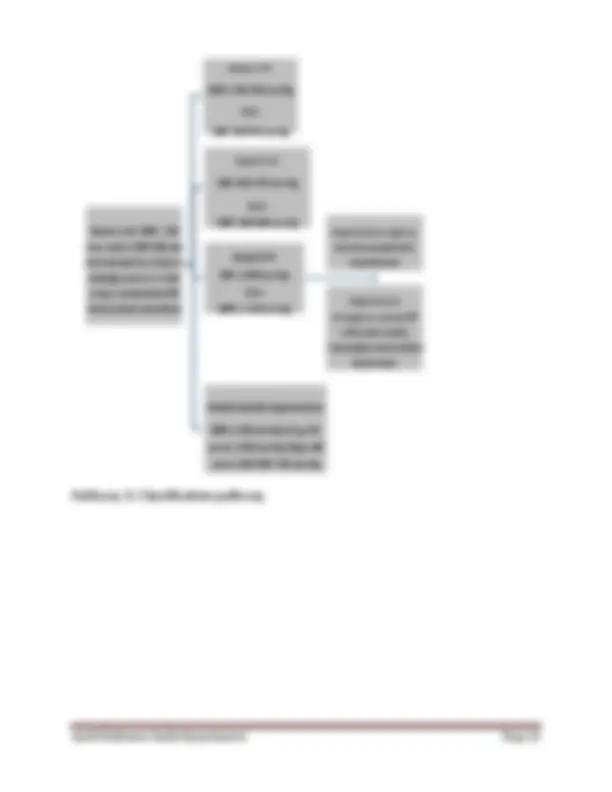
factors(apart from hypertension) : age ( > 55 years in men, 65 years in women), male gender, diabetes mellitus,smoking,obesity(including abdominal obesity), dyslipidemia(High LDL, Low HDL,High TG), impaired fasting glucose(FPG 100-125 mg/dl), family history of premature coronary artery disease. 3.2.2 Pragmatic approach to assessment of hypertensives in India : In the context of the Indian public health system, we suggest an approach which balances the needs of patients and the resources available at various levels and outline a pragmatic approaches to assessment – essential assessment in all patients with Grade 1 HT, desirable assessment in those with grade 2 HT or those with diabetes and/or proteinuria, and comprehensive assessment in those with Grade 3 HT, or those with diabetic complications, CKD, heart failure, or with a suspicion of secondary hypertension are suggested. This approach also takes into account the fact that some investigations like ECG for left ventricular hypertrophy have poor sensitivity , while there is insufficient evidence that a routine ophthalmoscopic examination is required for all patients with hypertension. On the other hand, patients with diabetes, symptomatic cardiovascular disease, smokers, obese, and those with proteinuria, which are all associated with greater cardiovascular risk can be identified even at the level of a primary health centre using a combination of clinical features (history and clinical examination) and investigations. Assessment of lipids is desirable in patients with hypertension, with a higher yield in those who are diabetics, obese and have cardiovascular disease. Patients can be referred to the community health centre for evaluation of lipids, but the need is not urgent. Essential assessment Should be done in all patients attending primary care facilities, also in patients with Grade 1 hypertension History and physical examination for risk factors (smoking, obesity, diet and exercise patterns, family history of premature CVD), clinical cardiovascular disease (angina, heart failure, stroke) Fasting capillary blood(FCG) or fasting plasma glucose (FPG). FCG > 126 mg/dl or FPG >126 mg/dl is abnormal and suggestive of diabetes. Abnormal fasting capillary glucose needs to be checked against a fasting plasma glucose obtained in the laboratory
4.2. Lifestyle modifications 4.2.1 Lifestyle measures including adopting a heart-healthy diet with reduced salt and saturated fat intake, stopping use of tobacco products , regular exercise and reduction of body weight in those who are obese, are part of management of all patients with hypertension. 4.2.1.1. These lifestyle measures may be sufficient for treatment of Grade 1 hypertension, may reduce the doses required for control of hypertension, and will also reduce the cardiovascular risk in all grades of hypertension. 4.2.1.2 A trial of lifestyle measures should be monitored for 1-3 months following diagnosis of Grade 1 hypertension. The lower range of durations should be considered in the presence of other risk factors like age, obesity, lipid levels, and smoking status. 4.3 Initiation of drug therapy 4.3.1 Drug therapy is indicated in patients with Grade 1 hypertension with
4.3.3.2.Drug therapy is initiated in patients with Grade 2 hypertension on confirmation of the diagnosis on repeat BP measurements in the visits subsequent to the initial visit when Grade 2 HT was first detected. 4.3.3.3.Drug therapy in patients with Grade 3 hypertension is initiated after repeat measurements in the initial visit confirm the severe elevation of the blood pressure. 4.4. Treatment goals for management of hypertension : 4.4.1 The current target for control of BP for patients under 80 years of age should be less than systolic blood pressure less than 140 mm and diastolic blood pressure less than 90 mm. 4.4.2 The current target for control of BP for patients 80 years or older should be less than 150 mm systolic and less than 90 mm diastolic. 4.4.3 A recent trial (SPRINT trial) in non-diabetic population at high cardiovascular risk has shown a reduction in cardiovascular mortality in patients in the intensive treatment group where the goal BP was less than 120 mm systolic and 80 mm diastolic. However this was accompanied by more than 2 fold increased frequency of serious adverse events and increase in serum creatinine. Based on the currently available evidence we do not recommend this lower target generally for physicians and patients in India, except for individual patients and physicians in situations who have agreed upon these targets and where close monitoring for adverse effects is feasible. 4.4.4 Current evidence based on trials of BP targets of <130 mm and < 85 mm diastolic in patients with diabetes have failed to show significant overall benefit on cardiovascular disease outcomes, and have been accompanied by increased frequency of serious adverse events. Therefore we currently recommend the standard BP target of <140 mm systolic and <90 mm in patients with diabetes in India. TARGET < 80 years: Systolic BP < 140mm Hg Diastolic BP < 90mm Hg
80 years: Systolic BP < 150mm Hg Diastolic BP < 90mm Hg Diabetics: Systolic BP < 140mm Hg Diastolic BP <90mm Hg
Clinical condition Drug to be preferred as first drugs Second drug if needed to achieve BP control Third drug if needed to achieve BP control Isolated systolic hypertension ( elderly) CCB/Thiazide Diuretic ACE Inhibitor* Thiazide diuretic + ACE Inhibitor+ CCB Hypertension and diabetes ACE inhibitor CCB or thiazide diuretic ACE inhibitor* + CCB+ thiazide diuretic Hypertension and chronic kidney disease(defined as albuminuria or an eGFR< 60 ml/min/1.73 m^2 for > 3 months) ACE inhibitorwhere close clinical and biochemical monitoring is possible. Otherwise CCB may be preferable CCB or thiazide diuretic (loop diuretic if eGFR is below 30 ml/min) ACE inhibitor +CCB+ thiazide diuretic Hypertension and previous myocardial infarction BB, ACE Inhibitor* CCB or diuretic Hypertension associated with heart failure Thiazide/ loop diuretic+ ACE Inhibitor+BB#+ Spironolactone Hypertension associated with previous stroke ACE inhibitor Diuretic or CCB ACE Inhibitor* +CCB+ diuretic Table 9 : Clinical conditions which may be associated in a patient with hypertension and the drugs to be preferred *Angiotensin receptor blockers (ARBs) may be used for this indication if there is intolerance to ACE inhibitors (cough, angioedema)Abbreviations: ACE inhibitor: angiotensin converting enzyme inhibitor; CCB, calcium channel blocker; BB, beta- blocker.Notes: Examples of representative drugs: ACE inhibitors - Enalapril, Calcium channel blockers-Amlodipine, Thiazide diuretic- Hydrochlorothiazide, Beta-blocker- Atenolol.#^ In patients with heart failure the preferred beta-blockers are metoprolol, carvedilol, bisoprolol. § Source: adapted from ref.(^21 ) Table 10 : Compelling and possible contraindications to the use of antihypertensive drugs
Drug Compelling contraindication Possible contraindication Diuretics Gout Metabolic syndrome, glucose intolerance, hypokalemia, hypercalcemia Beta-blockers Asthma, AV block (grade 2 or 3) Metabolic syndrome, glucose intolerance, chronic obstructive pulmonary disease Calcium channel blockers(dihydropyridines) Tachyarrhythmia, heart failure Calcium channel blockers(non- dihydropyridines) AV block (Grade 2 or 3),severe left ventricular dysfunction, heart failure ACE inhibitors Pregnancy Hyperkalemia Bilateral renal artery stenosis Women with childbearing potential Angiotensin receptor blockers Pregnancy Hyperkalemia Bilateral renal artery stenosis Women with childbearing potential Mineralocorticoid receptor antagonists ( e.g. spironolactone) Acute or severe renal failure (eGFR<30 ml/min) Abbreviations: AV, atrioventricular; eGFR, estimated glomerular filtration rate
Source: ref. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Blood pressure. 2013;22(4):193- 278.
4. 6 The treatment regimen and the use of combinations: 4.6.1 In patients with Grade 1 or Grade 2 hypertension, therapy can be initiated with one drug (CCBs, ACE inhibitors, thiazide diuretics) in combination with lifestyle modifications ( Step 1 in table 13). Average initial doses can be 5 mg of amlodipine, 5 mg of enalapril and 12.5 mg of hydrochlorothiazide. 4.6.2 In patients with Grade 3 hypertension, the therapy should be initiated with two drugs, in combination with lifestyle modifications ( Step 2 in table 13). The combinations can be calcium channel blocker (amlodipine) + ACE inhibitor (enalapril) or calcium channel blocker (amlodipine) + thiazide diuretic (hydrochlorothiazide) or ACE inhibitor (enalapril) + thiazide diuretic (hydrochlorothiazide). 4.6.3 The dose of drugs can be increased or a new drug added at approximately 2- to 4-week intervals. This frequency can be faster or slower depending on the clinical circumstances of the patient and the judgment of the practitioner. 4.6.4 The addition of a new drug in patients with Grade 1 or Grade 2 hypertension may be preferable to maximising the dose of the initial drug. In case a calcium channel blocker (amlodipine) has been used as initial therapy, the add-on drug can be ACE inhibitor (enalapril) or a thiazide diuretic. Similarly if ACE inhibitors have been used as initial therapy, a calcium channel blocker or a diuretic can be used as add on therapy. When amlodipine is used as an add-on therapy, the initial dose used should be 2.5 mg. Similarly if an ACE inhibitor like enalapril is added to a diuretic, the initial dose used may be 2.5 mg to avoid hypotension. 4.6.5. If the second drug in a usual dose also fails to reduce BP to target levels then the third class of drug previously unutilised should be added ( Step3 in table 13). An optimal 3 drug combination in case it is required is a calcium channel blocker with a low dose thiazide diuretic and an ACE inhibitor (e.g. amlodipine+ enalapril+ hydrochlorothiazide). 4.6.6. The preferred 2 drug combinations are combination of calcium channel blockers with ACE inhibitors, ACE inhibitors with low dose diuretics, and calcium channel blockers with low dose diuretics. 4.6.7. Prescription of a single pill combination of antihypertensive drugs in a defined proportion may be considered if available, after BP has been stabilised with a dose of two drugs given singly in the same proportion.
MANAGEMENT OF HYPERTENSION - target BP <140/90 mmHg in those < 80 years, 150/90 in those over 80 years. ALL PATIENTS REQUIRE LIFE-LONG LIFESTYLE MODIFICATION Dietary change to Heart-healthy diet– salt 5 6 g/day, low-fat diet Regular exercise Maintain weight – target BMI 18.5-22.9 kg/m^2 Stop smoking Patients with Grade 1 hypertension may require only lifestyle modification, which should be tried for 3 months. GRADE 1 HYPERTENSION (SBP 140-159 mm, DBP 90-99mm) with Inadequate control after 3 months of lifestyle modification OR more than 3 risk factors: Male,Age: men >55 years, women>65 years,smoking, obesity, including abdominal obesity Dyslipidaemia,impaired fasting glucose, family history of early coronary artery disease Drug therapy – A or C^1 or D Add second drug - A+C or C+D or A+D if response not adequate within 2-4 weeks Add third drug – A+C+D if response not adequate within 2-4 weeks GRADE 2 HYPERTENSION (SBP 160- 179 , DBP 100 - 109 ) Drug therapy – A or C or D Add second drug - A+C or C+D or A+D if response not adequate within 2-4 weeks Add third drug – A+C+D if response not adequate within 2-4 weeks GRADE 3 HYPERTENSION (SBP ≥180, DBP ≥110) Use two drugs - A+C or C+D or A+D Add third drug – A+C+D if response not adequate within 2-4 weeks ALL GRADES OF HYPERTENSION WITH ASSOCIATED CLINICAL CONDITIONS CAD: coronary artery disease - B+A^2 , C CHF: congestive heart failure - D+A+B, MRA CKD: chronic kidney disease – A or C or D^3 DM: diabetes mellitus – A or C, D Drugs are added only if they are required to achieve the target BP of <140/90 mm Hg (in patients <80 years old) or <150/90 mm Hg (in patients >80 years of age) Abbreviations : CAD : coronary artery disease, CHF : congestive heart failure, CKD : chronic kidney disease, DBP : diastolic blood pressure, DM : diabetes mellitus, SBP : systolic blood pressure, TOD: target organ damage. Drug classes: A : A ngiotensin converting enzyme (ACE) inhibitors, (e.g. enalapril) or Angiotensin II receptor blockers (ARBs) (e.g. losartan) if intolerance to ACEinhibitors, B : B eta-blockers (e.g. atenolol), C : C alcium channel blockers (e.g. amlodipine), D : thiazide d iuretics (e.g. hydrochorothiazide), MRA : mineralocorticoid receptor antagonist (e.g. spironolactone). Drug doses: Doses for initiation of therapy : A : enalapril 5 mg; B: Atenolol 50 mg; C: Amlodipine 5 mg ( 2.5 mg in elderly); D: Hydrochlorthiazide/Chlorthalidone 12. 5 mg. Add-on doses: A : enalapril 5 mg (reduce in elderly or in those on diuretics), C: amlodipine 2.5 mg, D: hydrochlorthiazide 12.5 mg Maximal doses: A : enalapril 20- 40 mg; B: Atenolol 100 mg C: Amlodipine 10 mg; D: Hydrochlorthiazide: 25 mg Footnotes : (^1) Calcium channel blockers are antihypertensives of choice in the elderly (> 60 years). (^2) Patients with CAD and history of myocardial infarction should receive both beta-blockers and ACE inhibitors 3 Patients with CKD may require loop diuretics if the glomerular filtration rate is low. Patients on ACE inhibitors will require monitoring of serum creatinine and potassium. Based on references: Hypertension: Clinical management of primary hypertension in adults NICE guidelines [CG127]. National Institute for HealthCare Excellence; 2011 Weber MA, Schiffrin EL, White WB, et al. The Journal of Clinical Hypertension. 2014;16(1):14-26.
Quick Reference Guide-Hypertension Page 20 Table 12: Initial and maximal doses for initiation and titration of therapy for Indian patients with hypertension: (source: adapted from ref ( 24 ), ( 70 ) and product monographs listed at health Canada www.health-sc.gc.ca) Drug class Low dose in certain situations Usual Initial dose suggested for Indian patients with hypertension Maximal dosage suggested for Indian patients with hypertension Doses per day Calcium channel blockers Dihydropyridines Amlodipine 2.5 mg* 5 mg 10 mg 1 Angiotensin converting enzyme inhibitors Enalapril 2.5 mg§^ 5 mg 10 - 20 mg 1 - 2 Lisinopril 5 mg 10 mg 1 Angiotensin receptor blockers Losartan 25 mg #^ 50 mg 100 mg 1 - 2 Telmisartan 40 mg 80 mg 1 Diuretics Thiazides 1 Hydrochlorothiazide 12.5 mg 25 mg 1 Thiazide-like Chlorthalidone 12.5 mg 25 mg 1 Beta-blockers Atenolol 25 mg 50 mg 100 mg 1 Metoprolol succinate 50 mg 100 mg 2 ***** Reduce dose of amlodipine to 2.5 mg once a day when it is started in low body weight elderly patients, and when amlodipine is added to another antihypertensive medication. § Reduce dose to enalapril 2.5 mg when it is used in elderly (>65 years) and when the patient has been on diuretic therapy.