









Study with the several resources on Docsity

Earn points by helping other students or get them with a premium plan


Prepare for your exams
Study with the several resources on Docsity

Earn points to download
Earn points by helping other students or get them with a premium plan
Community
Ask the community for help and clear up your study doubts
Discover the best universities in your country according to Docsity users
Free resources
Download our free guides on studying techniques, anxiety management strategies, and thesis advice from Docsity tutors
The programme aims to enable pharmacists to develop post graduate skills to gain „general level‟ pharmacist practitioner status.
Typology: Slides
1 / 16

This page cannot be seen from the preview
Don't miss anything!








1 PAF originally approved: 19 January 2011 PAF modified re: programme table: 17 February 2012
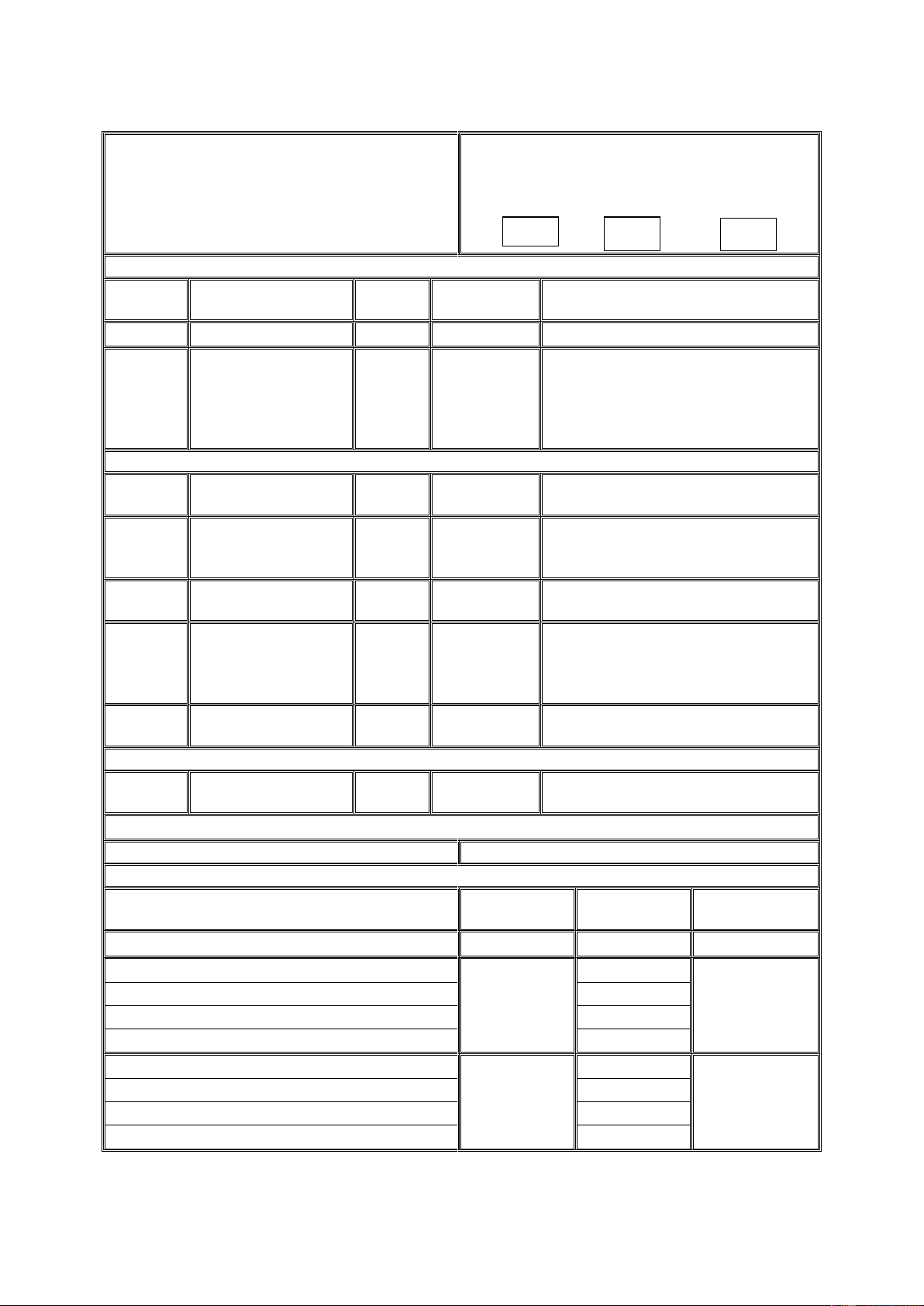
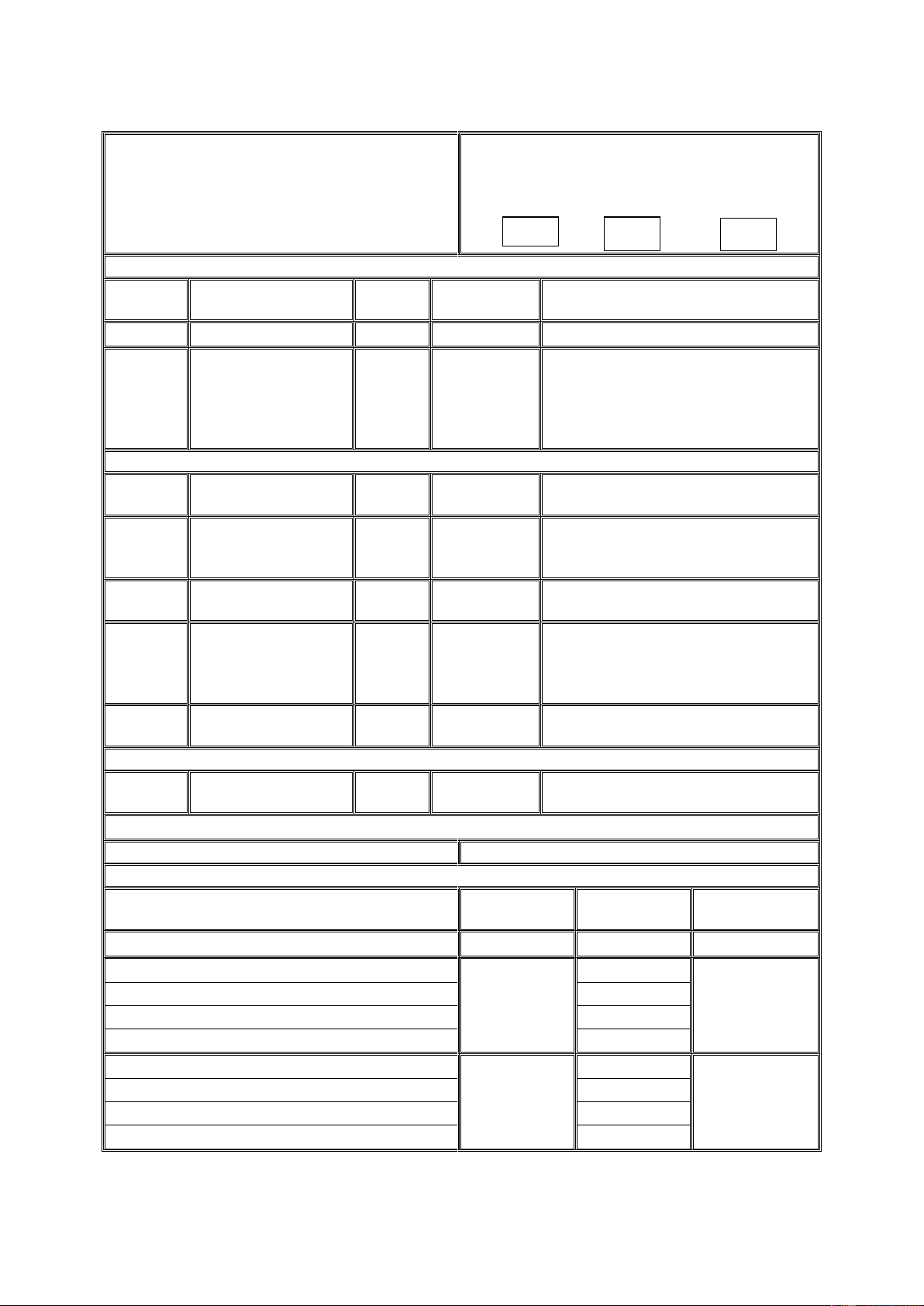
1. Programme title and designation Pharmacy practice
For undergraduate programmes only Single honours Joint Major/minor
2. Final award
Award Title Credit value
equivalent
Any special criteria
MSc Pharmacy Practice 180 90 N/A
MSc Pharmacy Practice (Prescribing)
180 90 Completion of the Practice Certificate in Independent Prescribing (7BBPM022) and any 15 credit modules and the Pharmacy Practice Dissertation Module.
3. Nested award
Award Title Credit value
equivalent
Any special criteria
PGCert In Independent Prescribing
60 30 To include completion of Practice Certificate in Independent Practice module (7BBPM022)
PGCert In Pharmacy Practice 60 30 To include completion of any four 15 credit modules
PGDip In Pharmacy Practice (Prescribing)
120 60 To include completion of the Practice Certificate in Independent Practice module (7BBPM022) and any four 15 credit modules
PGDip In Pharmacy Practice 120 60 To include the completion of any eight 15 credit modules
4. Exit award
Award Title Credit value
equivalent
Any special criteria
See above
5. Level in the qualifications framework M 6. Attendance
Full-time Part-time Distance learning Mode of attendance No Yes No Minimum length of programme
n/a n/a
PGCert 8 months
PGDip 16 months
MSc 24 months
Maximum length of programme
n/a n/a
PGCert 3 years
PGDip 4 years
MSc 6 years
2 PAF originally approved: 19 January 2011 PAF modified re: programme table: 17 February 2012
7. Awarding institution/body King‟s College London 8. Teaching institution King‟s College London 9. Proposing department Department of Pharmacy 10. Programme organiser and contact details
Dr. Sue C. Jones Department of Pharmacy Franklin-Wilkins Building Waterloo Campus Room 5.82, Extn. 4847 sue.jones@kcl.ac.uk
11. UCAS code (if appropriate) n/a 12. Relevant QAA subject benchmark/ professional and statutory body guidelines
n/a
13. Date of production of specification February^2010 14. Date of programme review March 2016
15 Educational aims of the programme i.e. what is the purpose if the programme and general statements about the learning that takes place over the duration of the programme
The programme aims to enable pharmacists to develop post graduate skills to gain „general level‟ pharmacist practitioner status. The purpose of the programme is to enable pharmacists to effectively develop and deliver modern patient centred pharmaceutical services within the primary care. Pharmacists will learn: to develop and demonstrate a reflective conceptual understanding of the issues and roles associated with complex clinical decision making an in-depth understanding across a broad range of the subjects relative to the professional roles and responsibilities of a pharmacist and contribute actively to the planning and delivery of patient focussed care in the National Health Service the knowledge, skills, competencies and proficiencies to meet the new regulations requirements for on-going revalidation by the General Pharmaceutical Council to provide safe and effective pharmacy services considered essential the skills required to undertake a research project that includes the construction of research questions, critical exploration and critical evaluation of outcomes appropriate to the development of pharmaceutical care.
16. Educational objectives of the programme/programme outcomes (as relevant to the SEEC Credit Level Descriptors) By the end of the programme the graduate will be able:
4 PAF originally approved: 19 January 2011 PAF modified re: programme table: 17 February 2012
Delivery of defined areas of practice as outlined in the local Primary Care Trust‟s published Pharmaceutical Needs Assessment and Joint Needs Assessment; Workforce development; Maximising the benefit of the community pharmacy contractual framework to support General Medical Practitioners‟ deliver their Quality and Outcomes Framework; Research methods, techniques for research and academic enquiry.
Practice assessment Plan and record (CPD record) Review of essential components of the community pharmacy contractual framework obligations including community pharmacy patient questionnaire, change management supported by practice audits and multi- disciplinary audits. Oral Presentation Written dissertation Poster presentation Research abstract
Skills and other attributes
Intellectual skills:
These are achieved through the following teaching/learning methods and strategies :
Intellectual skills set out in points 1 – 10 are developed through workshops, role play scenarios, seminar and tutorial sessions, oral and poster presentations.
Assessment :
Skills are assessed using a variety of methods including: Written examination Multiple Choice Questions (MCQ) Objective Structured Clinical Examination (OSCE) Critical review of therapeutic area Portfolio of Evidence to include performance assessment tools o CbD (Case based discussion) o MRCF (Medication Related Consultation Framework) o review of clinical interventions Business proposal to support a pharmacy practice development Therapeutic framework Medicines related risk framework Plan and record (CPD record) Review of essential components of the community pharmacy contractual framework obligations including community pharmacy patient
5 PAF originally approved: 19 January 2011 PAF modified re: programme table: 17 February 2012
questionnaire, change management supported by practice audits and multi- disciplinary audits. Oral Presentation Written dissertation Poster presentation Research abstract Student centred learning involving library based research, data retrieval and presentations will be encouraged to reinforce and enhance these skills.
Practical skills :
These are achieved through the following teaching/learning methods and strategies :
Subject practical skills are developed in a coordinated and progressive manner throughout the programme including workshop tutorials, computer-based sessions and in the work place when undertaking work-based evaluations. The skills associated with the development of research methods protocols are met during the sustained research project.
Reflective practitioner skills are developed throughout the programme using blended learning, the combination of taught and self directed learning using a range of delivery methods. Students will develop their learning supported by peer learning and peer review.
Pharmacy practice will be informed by evidence and patient evaluation. This will provide a coherent approach to supporting the development of reflective „general level‟ pharmacist practitioner. Critical analysis skills will be developed throughout the programme informed by metrics, audit, peer review and patient evaluation.
Assessment : A variety of assessment methods are used to assess skills, these may include: Written examination Multiple Choice Questions (MCQ) Objective Structured Clinical Examination (OSCE) Critical review of therapeutic area Portfolio of Evidence to include performance assessment tools o CbD (Case based discussion) o MRCF (Medication Related Consultation Framework)
7 PAF originally approved: 19 January 2011 PAF modified re: programme table: 17 February 2012
questionnaire, change management supported by practice audits and multi- disciplinary audits. Oral Presentation Written dissertation Poster presentation Research abstract
17. Statement of how the programme has been informed by the relevant subject benchmark statement(s)/professional and statutory body guidelines
The proposed programme structure will include the accredited Post-graduate Practice Certificate in Independent Prescribing (this has been approved by the Royal Pharmaceutical Society of Great Britain) and the commissioned module Oral Contraception Services module (this meets the clinical and corporate governance standards of Southwark Primary Care Trust and acts as the formal accreditation process for the enhanced service offered by community pharmacists within the community pharmacy contractual framework). There are no specific benchmark statements for this programme; however, attention has been placed upon the QAA benchmarking statements for pharmacy so that the programme and curriculum are informed by the specific subject knowledge, abilities and skills outlined in these statements and build on for postgraduate level. The programme has been developed informed by collaboration between Higher Education Intuitions in the South East of England supported by the Joint Programme Board, and incorporates changes and development requirements contained within the community pharmacy contractual framework and health policies. The programme will support the General Pharmaceutical Council standards underpinning the re-validation process.
18. In cases of joint honours programmes please provide a rationale for the particular subject combination, either educational or academic
n/a
Which is the lead department and/or school?
8 PAF originally approved: 19 January 2011 PAF modified re: programme table: 17 February 2012
1 9. Programme structure
Please complete the following table and, if appropriate to include joint, major/minor or other variations
Code =code of each module available for the programme Title = title of each module available for the programme, plus its credit level and credit value Status = please indicate whether the unit/module is introductory (I), core (Cr), compulsory (Cp), one or more of however many modules must be passed to progress (CrCp), (P) professional (i.e. module testing skills/ competency that has no credit level or value but is a professional body requirement) or optional (O) for each type of programme. For postgraduate programmes use the “single honours” column Pre requisite/Co-requisite =where appropriate please indicate whether the module is pre-requisite to another module or co-requisite by noting pre or co and the module code that is pre/co-requisite to. Assessment = please indicate in broad terms the assessment for the module eg written examinations, coursework (Note: the availability of optional modules may vary slightly from year to year, the following are the modules available at the commencement of the programme)
Code Title Credit level
Credit value
Status (I, Cr, CP, CrCP, P, O) for each type of module
Pre-requisite/Co- requisite (please note the module code)
Assessment
Single Joint Major/ minor
Single Joint Major / minor Part-time Study (this is a two year cycle of modules) 7TTY (KLI module)
Personal development and continuing professional development
7 15 O Coursework: critical account
Establishing professional & clinical practice within a pharmacy context
1 )Therapeutic review of two patients linked to scope of practice 2 ) Critical reflection of personal development plan
7BBPP004 Supporting patients with mental illness
10 PAF originally approved: 19 January 2011 PAF modified re: programme table: 17 February 2012
7BBPP013 Paediatric Pharmaceutical Care
7BBPP008 Service development in a pharmacy context
7BBPP005 Medicines and older people 7 15 O
1.Critical reflection of risk framework of a complex patient 2.Reflection of case summaries of clinical contributions for two complex patients
7TTY (KLI module)
Professional development in the workplace
work based assignment or equivalent
Delivering effective, patient-centred care in a pharmacy context
1.Design an informed adherence strategy to facilitate patient centred care 2.Demonstrate the application of the adherence strategy using a consultation framework 3.Oral presentation
Supporting self management of cardiovascular disease
11 PAF originally approved: 19 January 2011 PAF modified re: programme table: 17 February 2012
Supporting self management of respiratory disease
Supporting Self- Management of Contraception and Sexual Health
7BBPP011 Research Methods 7 15 O
Pharm acy practic e dissert ation
Module)
Fundamentals of Pedagogy 7 15 O Coursework
Module)
Management People in the Work Environment 7 15 O^ Coursework
7TTY (KLI Module)
Interprofessional Leadership and Learning 7 15 O^ Coursework
7TTY0 012 (KLI Module)
Models of Expertise 7 15 O Coursework
7TTY (KLI Module)
e-Pedagogy 7 15 O Coursework
13 PAF originally approved: 19 January 2011 PAF modified re: programme table: 17 February 2012
Other relevant information to explain the programme structure Please note that new students enrolling on the information provided on this section of the PAF will have these regulations stipulated throughout their programme of study. The only exception to this will be if there are changes made by Professional regulatory or Statutory Bodies that are notes to this programme.
Students who undertake the programme as full-time are expected to undertake the dissertation during the second year of their studies
14 PAF originally approved: 19 January 2011 PAF modified re: programme table: 17 February 2012
20. Marking criteria Pass marks and conditions for progression are as specified in the Academic Regulations for Taught Postgraduate Students established by King‟s College, London. 21. Will this Programme Board of Examiners report to an existing Board, and if so which one? If a new Programme Board of Examiners is to be set up please note name of Board here This programme has a board of examiners and will report to the Postgraduate Pharmacy Practice Exam Board. A board currently exists for the Practice Certificate in independent prescribing. 22. Please confirm that the process for nominating External Examiners has commenced, and if known, note whom the nominated External Examiner(s) may be
The external examiner will be Dr. Karen Hodson (Cardiff) And the intercollegiate examiner may be Professor Felicity Smith ((School of Pharmacy)
23. Particular features of the programme which help to reduce the barriers experienced by disabled students to ensure that the programme is accessible to all students who meet the entry requirements Admissions All students in receipt of an offer receive an information booklet on the support services offered by the College. All students receiving offers who have indicated they have a disability in their application receive a letter from the School Disability Adviser with her contact details and offering the applicant the opportunity to discuss their requirements.
Publicity and Module Booklets These clearly communicate the key skills that will be required during the programme, the content of each module, the intended teaching methods to be used and module status (core/compulsory/optional).
Teaching Methods A wide range of teaching methods is utilised (as demonstrated by box 17).
Assessment Advice has been taken from the Equality & Diversity Department to ensure assessment methods do not unfairly discriminate against students with disabilities. The College‟s Special Examination Assessment Committee (SEAC) considers requests for adjustments to assessment to take account of learning and/or physical disabilities. Module outlines specify the assessment methods that will be used and explain that SEAC will need to be notified about requests for alternative assessment methods. The form that the alternative assessment will take has been specified for each module in advance.
Feedback Feedback on the programme will be regularly collected from students about their learning experience. The information collected is used towards the on-going development and improvement of the programme.
16 PAF originally approved: 19 January 2011 PAF modified re: programme table: 17 February 2012
Nature of the involvement of external body
Description of the learning resources available at the off- campus location Oral hormonal contraception services: Clinical assessment portfolio (see document for further details). Doctor or nurse mentor with appropriate qualifications (for details see section 14 prerequisites). Clinical environment of providing access to clients requiring oral hormonal contraception services (see details on clinical environments above).
What mechanisms will be put in place to ensure the ongoing monitoring of the delivery of the module Oral hormonal contraception services: Clinical placement details submitted and reviewed by the module organiser for appropriateness as part of the application process via the course specific application form Student self assessment audit of the clinical placement is included as an element within the clinical assessment portfolio and submitted for assessment. Referral to the course team is required if audit indicates learning environment is not appropriate. Mentor‟s details submitted and reviewed by the module organiser for appropriateness as part of the application process via the course specific application form.
Please attach report of the visit to the off-campus location
5. Recognition of study or award of credit thorough off-campus study or placement – Please indicate how the time will be spent, the length of time out, the amount of credit and whether it is a compulsory or optional part of the programme
N/A Year abroad Year in employment Placement Other (please specify)
Time spent ……………………Credit amount…….Compulsory/optional………………….
6. Please provide a rationale for any such time outside the College, other than that which is a requirement of a professional or statutory body
7. Please give details if the programme requires validation or accreditation by a professional or statutory body
Name and address of PSB
N/A
Frequency of validation/ accreditation Date of next validation/ accreditation