








































Study with the several resources on Docsity

Earn points by helping other students or get them with a premium plan


Prepare for your exams
Study with the several resources on Docsity

Earn points to download
Earn points by helping other students or get them with a premium plan
Community
Ask the community for help and clear up your study doubts
Discover the best universities in your country according to Docsity users
Free resources
Download our free guides on studying techniques, anxiety management strategies, and thesis advice from Docsity tutors
NURS 2063 FINAL EXAM STUDY GUIDE
Typology: Exams
1 / 49

This page cannot be seen from the preview
Don't miss anything!







































Final Exam Concept Guide Know the Etiology, Signs/Symptoms, Diagnosis/Diagnostics, Clinical Manifestation, Risks, Treatment and Complications for the following: ▪ Gastritis Gastritis – inflammation of the stomach lining Acute Gastritis – (just acquired) ingestion of toxins, alcohol, aspirin or other irritating substances Chronic - 2 months to become chronic Triggers of Gastritis: Alcohol, caffeine, autoimmune disease, viral or bacteria Chronic Gastritis: H Pylori is always a factor H Pylori goes very deep in the lining of the stomach and It causes persistent inflammation S/S: N/V – Anorexia- postcranial discomfort Post Cranial Discomfort - after eating- goes away and come back 1- hrs Gastritis- hematemesis- blood in the vomit- coffee brown color Treatment: Treat H pylori treat GERD, change lifestyle, PPI ▪ Peptic Ulcer Disease Inflammation and ulceration in the stomach (acid and pepsin) Gastric: stomach location Duodenal: duodenal location PUD is a complication of Gastritis PUD is caused by aspirin, H pylori, Nsaids, Stress, Smoking S/S Gastric N/V Anorexia Chest discomfort, asymptotic, Dyspepsia Duodenal – normal weight Biggest complication of PUD - GI bleeding due to Ulcer perforation- hole in the lining and bleed It is life-threatening if it keep bleeding (Anemic, electrolytes imbalance (losing volume) Duodenal – Blood in the stool – black and tarry Bleeding profusely-frank with cloth Hematemesis- Bleeding in vomiting Treatment: Cortery of perforation, treatment of H. pylori, PPI, Cessation of smoking ▪ Ulcerative Colitis and Crohn’s the difference in the complications Complication in UC Malnutrition – dehydration, increased risk factor of colon cancer 7-10 yrs, rarely in megacolon Complication of Chron- Fistulas, perianal fissures, abscesses. The risk of colorectal cancer ▪ Bowel Obstruction Manifestations Obstructions in the jejunal area: Vomiting, dehydration, electrolyte depletion Obstructions of the distal portion of the small bowl or ileum, dehydration to hypovolemic schock Obstructions of the colon: Massive gas distention Blockage of the colon by a tumor is the most common cause of colonic obstruction and
perforation of the bowel wall adjacent to the tumor. ▪ What percentage of the pancreas is dedicated to endocrine functions? Only 5% ▪ Pancreatic Cancer Pancreatic Cancer – 2% of all cancers Ranked 4th^ among death in all malignancies Risk Factors; cigarette smoking, obesity S/S; head: Jaundice, malabsorption, weight loss tail: Abd pain, nausea’ ▪ Hepatic Encephalopathy is due to? Hepatic encephalopathy is a decline in brain function due to severe liver disease
Lower mortalty and morbidity rates Control pains VS RISKS Electrolytes imbalance (potassium and sodium) -need to check hyper or hypo
Low blood pressure (have to check vitals before and after) Risk for infection Long-term mobidity Life threatening Cardiovascular disease remained the most common cause of death in ESRD patient ▪ Acute Kidney Injury- Three phases- Prodromal- Oliguric- Postoliguric Prodomal Phase
o • Distributive shock (neurogenic, anaphylactic, septic) o • Third-spacing and edema o • Decreased cardiac output ▪ • Cardiogenic shock ▪ • Dysrhythmias ▪ • Cardiac tamponade ▪ • Heart failure ▪ • Myocardial infarction
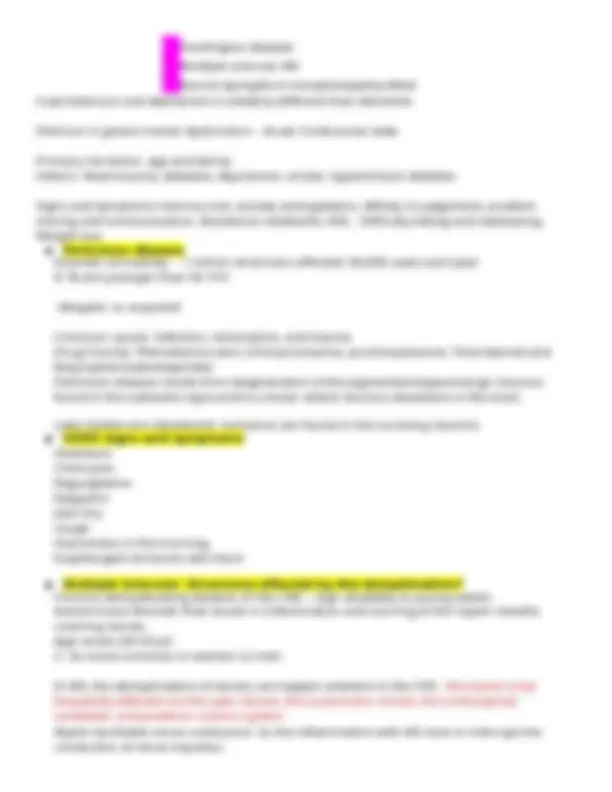
▪ What is the Glomerelus? ▪ It is a segment of nephron that filters fluid from blood into Bowman capsule, prevents passage of blood cells and proteins. ▪ What is Glomerulonephritis? ▪ An assortment of immune-mediated conditions that produce inflammation of the glomeruli. ▪ Diabetes Type I and Type II Type 1: Destruction of the B cells of the pancreas results in absolute insulin deficiency 5-20 yrs Chromosone 6 Type 2: Most common form of DM – Insulin resistance and B cells dysfunction lead to a resistance lack of insulin Risk factor: Female sex, obesity, and sedentary lifestyle Risk factor: non Caucasian, elderly ▪ Poly’s of Diabetes ▪ 3 P : Polyuria, Polyphagia, Polydipsia ▪ Cushing’s Syndrome characterized by Cushing Adrenocortical Syndrome Insufficiency Truncal obesity Moon face Dorsocervical fat pad Hirsutism Muscle wasting Striae Petechiae Glucose intoleranc e Hypertension Hypokalemia Weakness Hypotension Hypoglycemia Hyperpigmentatio n (Addison disease) Hyperkalemia Weight loss ▪ Traumatic Brain Injury ➢ Traumatic brain injury (TBI) refers to injuries of brain tissues sustained as a consequence of trauma ➢ Traumatic brain injury == head injury ➢ Injuries to the cranials =N not always brain injury ➢ TBI is the leading cause of death and disability in the U.S. 50,000 + yr ➢ Causes TBI (falls, sports injuries, firearms, and transportation-related trauma) ➢ Fall majority for 0-4 or 65+, motor vehicle TBI – 14-24 yr. Men are more likely to die
➢ Severity of TBI is classified by Glasgow coma scale (CGS) (standardized tool developed for the purpose assessing the LOC in acutely brain-injured patients. To evaluate patient with an altered LO ➢ Glasgow coma scale: Mild score (13-15), Moderate (9-12), severe (8 – below) ➢ Primary injury- initial trauma injury on brain cells
- Focal injuries (coup) - Polar injuries (coup contrecoup) - Diffuse injury In addition, as location, Primary Injury can also differentiated by Mechanism of injury - Concussion - Contusion - Intracranial hematoma. Concussion also known as Mild traumatic brain injury (MTBI) most common for military and athletes. Alterations or LOC ≤ 30 mn but no evidence of brain damage on CT. Symptoms: Headache, n/v, dizziness, fatigue, blurred vision, cognitive, emotional disturbances Contusion CT or MRI reveals area of Brain Tissue damage (necrosis, laceration, bruising) Intracranial hematoma: Localized collection of blood within the cranium. Three types; Epidural, subdural, subachnoid. Secondary Injury : Body’s response to initial injury may cause more harm than the initial injury. Can cause: Ischemia, hypoxic events, vasogenic/neurogenic edema, and other processes that leads to brain swelling and increased ICP. Treatment: Cardiopulmonary stabilization. Radiologic screening, maintenance of normal body temperature or mild hypothermia, normal PaCO2, normal glucose level and noema intravascular volume recommended. Acutely elevated ICP, mannitol(osmotic diuretic) sedation, hypothermia and mild hyperventilation. ▪ Reperfusion Injury- Definition Reperfusion injury is the secondary injury that occurs after reestablishing blood flow ▪ Increased Cranial Pressure- ICP ▪ ICP is the pressure exerted by the contents of the cranium and normal ranges from 0-15 mmhg The volume of the cranium nerve is made up 3 parts: brain tissue, cerebrospinal, blood Monroe-kellie hypothesis – the relationship between the 3 components of cranium Compliance – the ability to accommodate changes in volume w/o sign. Increase in pressure The most common causes of ICP: stroke, trauma and tumors ▪ Most sensitive indicator of altered brain function? A change in Level of consciousness LOC is one of the most sensitive indicators of altered brain function ▪ Assessment of the brainstem function- How do you assess it? Pupil light reflex Oculovestibular reflex Corneal reflex ▪ CVA- Types and causes Transient ischemic attack (TIA) – Episodes of stroke s/s with a duration of less than 24 hr and less
than1hr (30% pt with stroke have prior TIA) Ischemic stroke- Sudden occlusion of cerebral artery secondary to thrombus formation/embolization
- Thrombotic strokes: atherosclerosis and hypercoagulable states - Embolic strokes: cardiac sources
- Normal-pressure hydrocephalus - Parkinson disease - Lewy body disease
- Huntington disease - Multiple sclerosis MS - Bocine Spongiform encephalopathy (Mad Cow) Delerium and depression in elederly different than dementia Delirium in global mental dysfunction – Acute Confusional state Primary risk factor: age and family Others: Head trauma, diabetes, depression, stroke, hypertension diabetes Signs and Symptoms memory lost, anxiety and agitation, diffulty in judgement, problem solving and communication. Assistance needed for ADL. Difficulty eating and swallowing. Weight loss ▪ Parkinson disease Disorder of mobility - 1 million americans affected. 60,000 cases each year 4 % are younger than 50 Y/O idiopatic or acquired Common causes: Infection, intoxication, and trauma Drug Toxicity: Phenotiazine class: (Chlorpromazine, prochlorperazine, Thioridazine) and Butyrophenone(haloperidol) Parkinson disease results from degeneration of the pigmented dopaminergic neurons found in the subtantia nigra and to a lesser extent neurons elsewhere in the brain. Lewy bodies are cytoplasmic inclusions are found in the surviving neurons. ▪ GERD signs and symptoms Heartburn Chest pain Regurgitation Epigastric pain Dry cough Hoarseness in the morning Esapheogeal strictures with Gerd ▪ Multiple Sclerosis- Structures effected by the demyelination? Chronic demyelinating disease of the CNS – sign disability in young adults Autoimmune disorder that results in inflammation and scarring of the myelin sheaths covering nerves. Age onset (20-50 yr) 2 -3x more common in women vs men In MS, the demyelination of nerves can happen anwhere in the CNS. Structures most frequently affected are the optic nerves, the oculomotor nerves, the corticospinal, cerebellar, and posterior column system. Myelin facilitates nerve conduction. So the inflammation with MS slow or interrupt the conduction of nerve impulses.
Flexion injury with tearing of the posterior ligaments and dislocation is the most unstable injury and is aften associated with severe neurologic deficits Hyperextension injury is the most common S/S complete loss of function below the level of injury , Spinal shock (a few hrs) Flaccid paralysis of all skeletal muscles. Loss of all spinal reflexes, loss of pain, proprioception and other sensations, bowel and bladder dysfunction with paralytic ileus, loss of thermoregulation. Bradycardia, hypotension ▪ How to treat Spinal Cord Injuries Stabilization of the spinal vertebra (to prevent further trauma to spinal cord) Sugery – internal fixation or external fixation and bracing Surgery within 24 hrs if cord compression Use od high-dose methylprednisolone (1st^ 8 hrs) (controversial method) Removing or alleviating the painful stimuli Use od adrenergic receptor-blocking medication to manage hypertensive crisis Prevent respiratory and urinary tract infections Skin pressure sores Septicemia and fecal impaction ▪ Hypoventilation build up what? Hypoventilation causes build up of acid (acidosis) and too little oxygen in the blood. Hypoventilation occurs when delivery of air to the alveoli is insufficient to meet the need to provide O2 and remove CO2.
- Decrease rate and depth of respiration - Results in increased PaCO2 ≥ 45 mm Hg - Hypoxemia – increased alveolar CO ▪ Causes: drugs (morphines, barbiturates) , obesity (Pickwickian syndrome, myasthenia gravis, obstructive sleep apnea, chest wall damage. ▪ Normal ABG’s- Only must know normal values pH 7.35-7. PaCO 2 35-45 mm Hg PaO 2 80-100% HCO 3 22-26 mEq/L SaO 2 95-100% ▪ Acute Respiratory Failure- the goal of treatment Maintaining ventilatory support by maintaining airway patency and ensuring adequate alveolar is the primary goal of therapy. Mechanical ventilation
Management of the underlying cause. ▪ Virchow’s Triad of PE
Embolism Typ Cause e Thrombotic Blood clots develop in venous system, predominantly in thighs and legs Fat Globules of fat secondary to fractures of pelvis or long bones Amniotic fluid Collections of fluid, hair, or other debris related to complicated labor, especially in olde multiparous women Air Venous access through IV catheters Tumor Fragments from malignant tissue Foreign material Foreign bodies (bullets, sutures, catheter tips, orally prepared medications injected IV) Septic Infected tissue or related substances (fungal/bacterial) Parasitic Parasites present in lung vasculature ▪ Asthma- definition Asthma is complex lung disease and associated with the release of inflammatory chemicals from mast cells in the airways. Asthma is a lung disease characterized by:
- airway obstruction that is reversible (to some patients) - airway inflammation - increased airway reactivity to a variety of stimuli Mast cell release are IgE (immunoglobin E) mediated for both extrinsic and intrinsic asthma. Extrinsic Asthma: Allergies, family hx of the disease. Positive reaction to environmental triggers. Intrinsic Asthma: Respiratory Tract infections and psychological factors(harder to treat)
▪ Exercise-Induced Asthma is due to? Exercise-induced asthma is due to Running, jogging, bicycling. Bronchospasm occurs within 3 min after exercise and usually resolve in 60 minute. ▪ Acute and Chronic Bronchitis Acute Bronchitis is an acute inflammation of the trachea and bronchi. 80% of the 12 mil cases per yr in UD. o Influenza Virus A or B o Parainfluenza Virus o respiratory syncytial virus o Coronavirus o Rhinovirus o Coxsackie virus o Adenovirus o Streptococcus pneumoniae o Hemophilus influenza o Mycoplasma o Moraxella o Chlamydia pneumoniae (heat, smoke inhalation, inhalation of irritant chemicals) Risk factors: smokers, young children, elderly -winter months) Pathogenesis: The airways become inflamed and narrowed from capillary dilation, swelling from exudation of fluid, infiltration with inflammatory cells. S/S mild and self-limiting: - low-grade fever
- substernal chest discomfort - sore throat - postnasal drip - fatigue Associated inflammation of the larynx and trachea produces croup syndrome Diagnosis: Clinical presentation- onset of the cough. Treatment: Antibiotic therapy for bacterial infection Viral infection resolved spontaneously in most normal healthy person Primary goal is symptom management with antitussive agents – beta-2 agonists and bronchodilatoes Codeine-containing medication are helpful Non-pharmacologic: increase fluid intake, avoid smoke, use vaporizer in bedroom Chronic Bronchitis: Major causes of chronic bronchitis are: - Cigarette smoking (90 %) - Repeated airway infections - Genetic predisposition - Inhalation of physical or chemical irritants Chronic Bronchitis: Type B COPD Diagnosed: Symptomatically by hypersecretion of bronchial mucus and a chronic or recurrent productive cough of more than 3 months duration and occurring each year for 2