Download Outcomes & Complications of Minimally Invasive Esophagectomy: Duke & Pitt Univ. and more Slides Oncology in PDF only on Docsity!
Duke Masters of Minimally Invasive Thoracic Surgery Orlando, FL
September 17, 2016
Session V: Minimally Invasive Esophageal Surgery
Minimally Invasive Esophagectomy
James D. Luketich MD, FACS Henry T. Bahnson Professor and Chairman, Department of Cardiothoracic Surgery University of Pittsburgh Medical Center
Overview
- Background information
- Definition of a Minimally Invasive esophagectomy
- Evolution of technique
- Esophagectomy: Results of MIE
Trends in esophageal adenocarcinoma
incidence and mortality
Hur C et al. Cancer Dec 2012
Surgical Resection
Mortality from Esophagectomy in the U.S.
- National Medicare data base assessed outcomes from
a variety of surgical procedures
- Esophagectomy mortality ranged from 8.1% at high-
volume hospital to as high as 23% at low-volume hospitals (NEJM 2002)
- Published series from experienced centers lower this
to less than 5%, significant morbidity
- Less invasive approaches may help Surgeons to lower
morbidity
Early on Minimally Invasive Esophagectomy Lacked a Consistent Minimally Invasive Approach, What is a Minimally Invasive Esophagectomy?
- Right VATS, laparotomy and neck incision
- Laparotomy for gastric mobilization, thoracoscopic esophagectomy and intrathoracic anastomosis
- Laparoscopic gastric mobilization, thoracotomy with intrathoracic anastomosis
- Thoracoscopic esophagectomy, laparoscopic hand-assisted
- Totally laparoscopic mobilization, esophagectomy with neck anastomosis (Transhiatal)
- No advantages noted at that time, but clearly no consistent approach had emerged Our Approaches: totally laparoscopic/thoracoscopic
- Thoracoscopic esophagectomy, laparoscopic gastric mobilization and cervical anastomosis (McKeown)
- Laparoscopic gastric mobilization, thoracoscopy with intrathoracic anastomosis (Ivor Lewis)
Law and Wong: Lancet Oncology 2002
Operative Approaches
Initial Experience
- Laparoscopic transhiatal esophagectomy with
cervical anastomosis (n=9)
- Laparoscopic mobilization with right thoracotomy
(n=8)
- Laparoscopic and thoracoscopic esophagectomy
(n=59)
- Four conversions to open
- All secondary to adhesions
- No emergent conversions
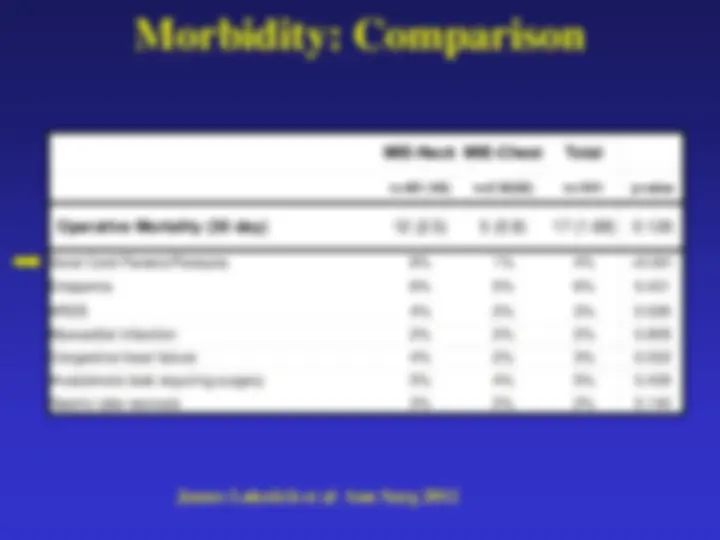
Major Complications (24%)
- Mortality: zero in first 77, 0
- Anastomotic leaks (n=7, 9%)
- Hypopharyngeal perforation (1)
- Tracheal tear post-op day 6 (1)
- ARDS (2)
- Permanent recurrent laryngeal nerve injury (n=2, 2.6%)
- Chylothorax (n=3, 3.9%)
- pyloric leak (1)
- pyloric stenosis requiring laparoscopic pyloroplasty (3)
- Partial necrosis of gastric tube (3)
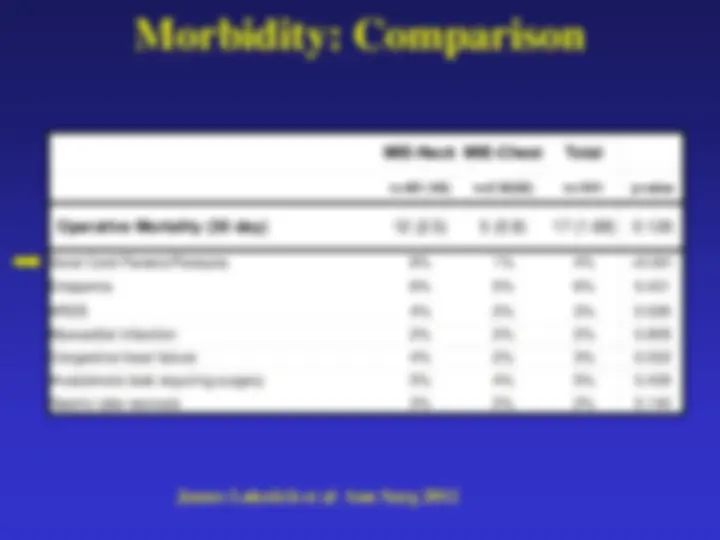
Luketich Series^ Orringer Series
Long-Term Results: Local
Recurrence Rates After MIE in
Pittsburgh
- 70 patients with esophageal cancer with documented N disease by lap staging
- Three cycles of chemotherapy followed by MIE with 2-filed lymph node dissection
- Oncologic outcomes:
- 5-year survival 35%
- At a median follow-up of over 40 months, local recurrence only in less than 5%
- Distant recurrence, primarily lung, liver, lung in 60%
- Lerut: 5% local recurrence rate after en bloc resection
Luketich, et al. Annals of Thoracic Surgery 2008
Technique: Laparoscopic-Transhiatal
versus thoracoscopic/laparoscopic
- Lap-THE:
- PRO:
- No repositioning pt
- No single lung ventilation
- CON:
- small working space
- Limited access to thoracic nodes
- Gastric tip ischemia
- RLN injury
- Lap/VATS:
- PRO:
- better exposure /dissection of mediastinum
- Better esophageal margins -? Survival/local recurrence benefit
- CON:
- repositioning required
- double lumen tube required
- Delayed abdominal assessment
- Gastric tip ischemia
- Gastric margins
- RLN injury
- MIE Ivor Lewis:
- PRO:
- pros of lap/vats
- No pharyngeal/RLN issues
- Less gastric tip ischemia
- Larger diameter anastomosis,
- less strictures
- Better gastric margins
- CON:
- Esophageal margins (SCC, or high Barrett’s
- Technical challenge of VATS anastomosis
N=15, initial approach N=>500 N=>700 current approach
Methods: Initial Series (n=222)
- Initial selection included only T-1 tumors and high-grade dysplasia
- As experience was gained, T2 (n=71) and T3N1(n=81) included
- Selection: resectable tumor by EUS and CT scanning, laparoscopic staging if questionable
- Prospective data base of standard outcomes
- Two quality of life (QOL) instruments
- SF-
- Heartburn-related QOL James Luketich et al Ann Surg 2003
Quality of Life Results
- SF-36 Global QOL
- Physical Component Score: 44 post-op, no significant difference compared to pre-op values or age-matched norms
- Mental Component score: 51 post-op, no significant difference compared to pre-op values or age-matched norms
- Heartburn-Related QOL
- Post-op score 4.6 consistent with normal population score
- Only 4% of patients had a post-op score in the severe reflux range (>15)
Laparoscopic Port Placement
Self-retaining liver
retractor
4 5-mm ports
one 10-mm port
Mobilization of Stomach
- Handle the stomach gently
- Division of the omentum and omental branches of
the gastroepiploic artery
- Avoid injury to the gastroepiploic arcade
- Avoid injury to the greater curvature of the
stomach while dividing the short gastrics
Creation of the gastric tube
- Construct narrow tube, 3-4 cm
- Begin 3-4 cm above pylorus
- Run staple line parallel to the line of the short gastrics
- Keep stomach on slight “stretch” while applying stapler
- Minimize trauma to the actual new conduit, “no touch”
technique