Download CLINICAL DOCUMENTATION GUIDE and more Study Guides, Projects, Research Nursing in PDF only on Docsity!
CLINICAL
DOCUMENTATION
GUIDE
January 2022
BEHAVIORAL HEALTH AND RECOVERY SERVICES
CONTENTS
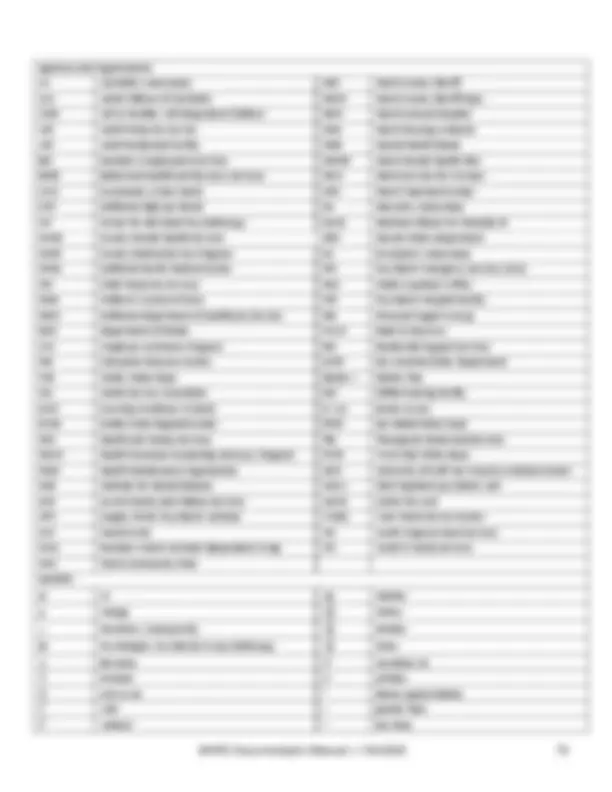
GENERAL PRINCIPLES OF DOCUMENTATION AND AUTHORIZATION
TIMEFRAMES
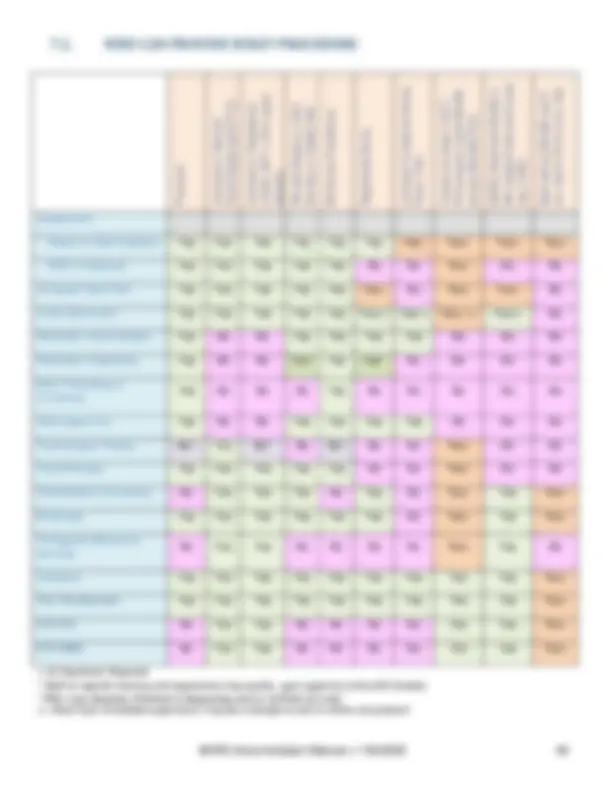
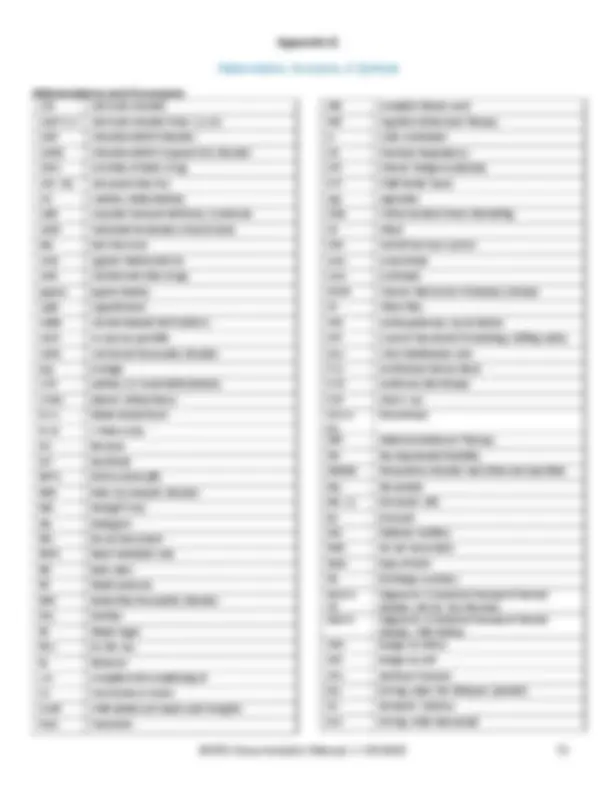
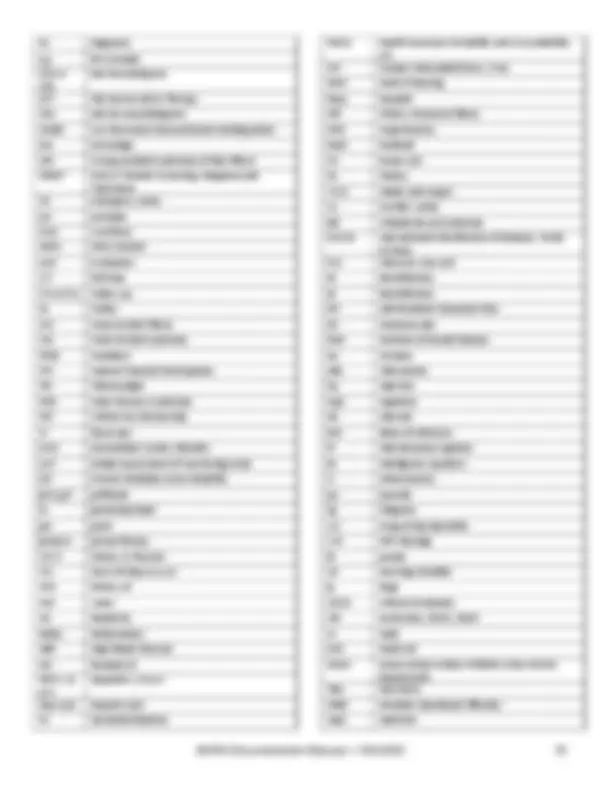
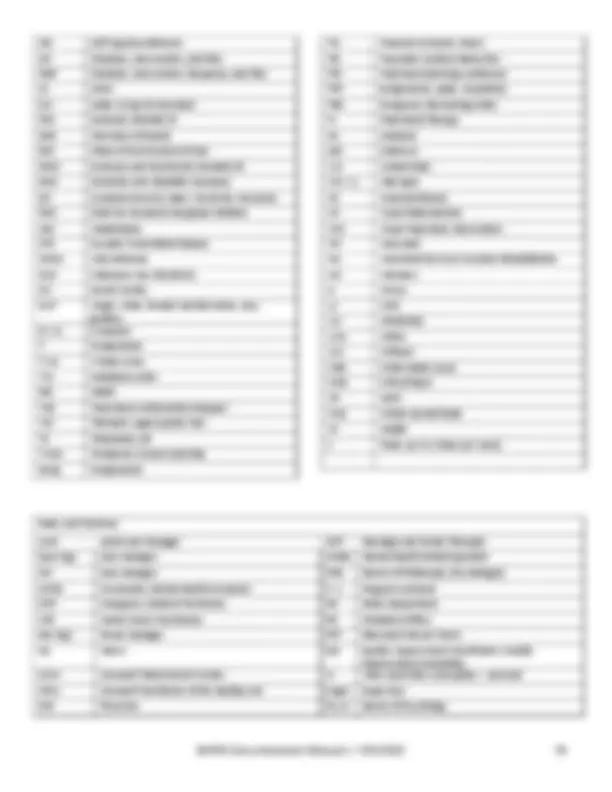
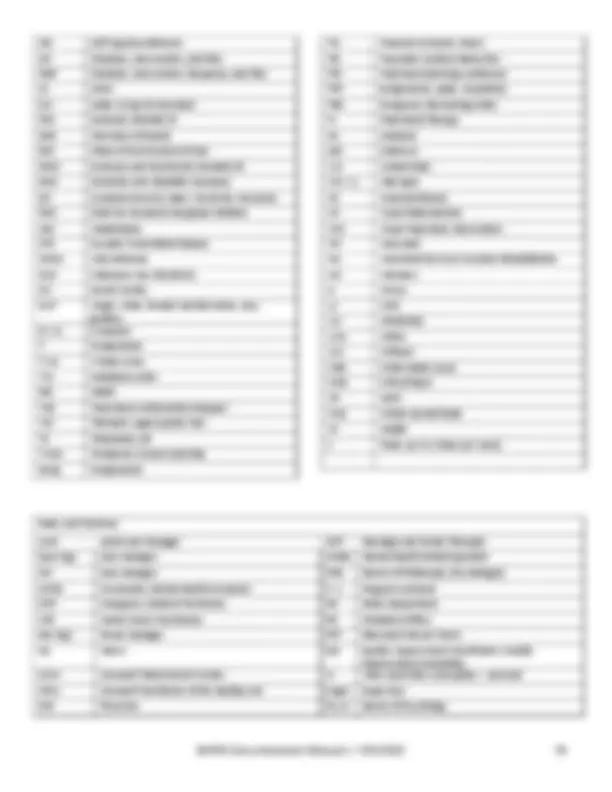
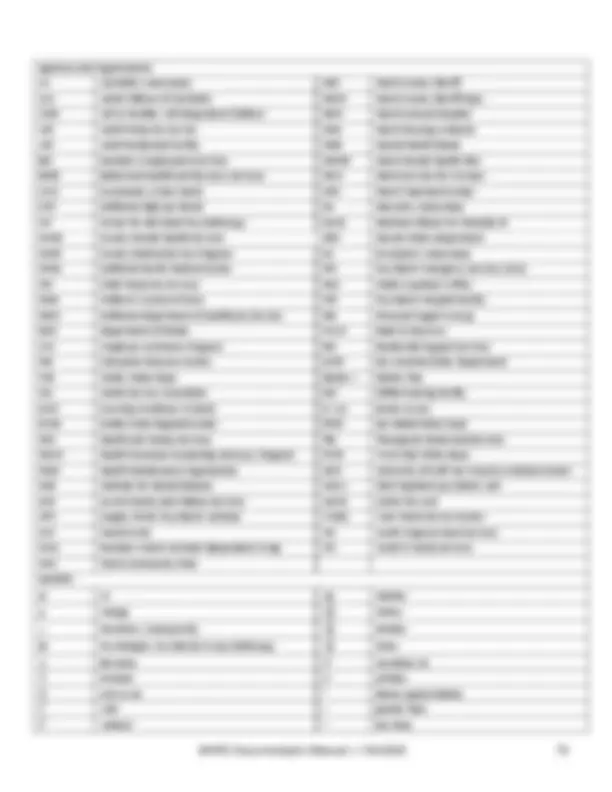
7.2 Who Can Provide What Procedure 46 7.3 Utilization Review 47 8 INFORMED CONSENT 48 8 .1 Minor Consent 48 8 .2 Medication Consent 51 8.3 Authorization to Exchange PHI 51 9 DOCUMENTATION REQUIREMENTS FOR SPECIFIC PROGRAM TYPES 53 9.1 Medication Clinic Documentation 53 9.2 Full-Service Partnership (FSP) Documentation 55 10 EXAMPLES 57 10 .1 Examples of Strengths 57 10 .2 Examples of Intervention Words 57 10 .3 Examples of Intervention Words for Specific Psychiatric Symptoms, Conditions 58 10 .4 Examples of Progress Notes 62 APPENDICES A Glossary B Title 9 service definitions C Coordinated care plan (CP) guideline D E F G BHRS Checklist for Documentation Abbreviations Lockout Assistant Changes for January 2022 & Revision History
1.1. WHY DO WE HAVE THIS MANUAL? As a behavioral health system, The Marin Behavioral Health and Recovery Services (BHRS) is committed to delivering client and family driven care. It is important that our service providers understand and embrace this philosophy. Client centered care has been recognized as a best practice in behavioral health. “All services and programs designed for persons with mental disabilities should be consumer centered, in recognition of varying individual goals, diverse needs, concerns, strengths, motivations, and disabilities.” Client centered care involves putting the consumer in the driver’s seat of the care they are receiving. There’s a saying throughout the healthcare industry that “if it isn’t documented, it didn’t happen.” In order to give evidence that the services that BHRS provides reflect the values stated above, good documentation practices need to be followed. This manual has been developed as a resource for providers of BHRS. It outlines documentation standards and practices required within the Children, Youth and Family System of Care, Adult/Older Adult System of Care, contract providers, and Substance Use Services. It serves to ensure that providers within BHRS meet regulatory and compliance standards of competency, accuracy, and integrity in the provision and documentation of their services. While this manual is not specific to any particular electronic medical record system, there are many specific items that refer to Clinician’s Gateway (CG). Where this is the case, it is usually stated as “In CG…” As with any manual that incorporates policies and regulations, updates will need to be made as these policies and regulations change. When updates are distributed, please be sure to replace copies or sections that have been downloaded or printed.
Please note that this is primarily a CLINICAL documentation guide, i.e., the main focus through this manual
is the clinical documentation in the medical record. There are other required documents which are more
administrative. These are included in Appendix E.
Sources of Information
This Clinical Documentation Guide is to be used as a reference guide and is not a definitive single source of
information regarding chart documentation requirements. This manual includes information based on the
following sources: Code of Federal Regulations (CFR) 45 and 42, the California Code of Regulations (CCR)
Title 9, the California Department of Health Care Services’ (DHCS) Letters and Information Notices, American
Health Information Management Association (AHIMA), California Advancing and Innovating Medi-Cal
(CalAIM) initiative, the Marin County Behavioral Health and Recovery Services (BHRS) policies & procedures,
directives, and memos; and the Quality Improvement Program’s interpretation and determination of
documentation standards. Note that many policies may be titled under BHRS’ previous name, MHSUS. As
policies are updated or revised, they will be renamed BHRS policies.
Suggestions and Feedback
Suggestions and feedback for enhancements, improvements, or clarifications to this manual are welcome.
Please send feedback to BHRSQM@marincounty.org.
Chapter 1. INTRODUCTION/COMPLIANCE
2.1. General Principles of Documentation
- All Providers must refer and adhere to BHRS-25, Documentation Standards for Outpatient Specialty Mental Health Services.
- Until the EHR is completely electronic; BHRS continues to maintain a hybrid health record system, which includes both paper-based and electronic documents. For new client admission and re-admission in Clinician’s Gateway, the hybrid health record continues to include chart forms that require client’s signature until signature pads and/or scanning capabilities become available system wide.
- All Providers must use BHRS approved forms or an approved electronic health record system for documentation. BHRS Contract Providers must incorporate all BHRS required documentation elements as referenced in this Manual and BHRS 25 policy.
- Required documents include an accurate Assessment, Client Plan, and Ongoing Care Notes (Progress Notes). Remember that the medical records, both electronic and paper, are legal documents.
- Only services that have been entered into CG, or for programs not using CG, services documented with progress notes, can be claimed.
- All services shall be provided by staff within the scope of practice of the individual delivering service. Clinicians will follow specific scope of practice requirements determined by regulations, including those of the governing boards of the applicable licenses.
- Progress notes should provide enough detail so that auditors and other service providers can easily ascertain the client’s status and needs and understand why the service was provided without having to refer to previous progress notes. Remember the Golden Thread when writing notes. This is the consistent presentation of relevant clinical information throughout all documentation for a client. Each note should lead into the next, creating a comprehensive story of the client’s progress through treatment.
- Each progress note must show that the service was medically necessary by documenting that it was reasonable and necessary to protect life, to prevent significant illness or significant disability, or to alleviate severe pain. In order to demonstrate medical necessity, progress notes should clearly identify the type of service provided and how the intervention addresses the client’s presenting condition. Clinicians can solidify the medical necessity of a service by documenting how the intervention provided relates to the clinical goals or mental health condition written in the client plan. Progress notes become a medically necessary service when the intervention provided attempts to reduce a functional impairment caused by a symptom of a diagnosis.
- It is crucial that the staff providing the service records the correct procedure for the service provided and that the documentation supports and substantiates this service. In order for Marin County to receive the correct reimbursement for services provided, clinicians must ensure that they choose the correct procedure for the correct Program Facility/Program and for the correct client. Chapter 2. GENERAL PRINCIPLES OF DOCUMENTATION AND AUTHORIZATION TIMEFRAMES
- Primary Total Time should be noted on each progress note. Primary total time is the time spent face-to-face with client plus any administrative time (e.g., documentation time and travel time to and from site, if applicable). Please remember to bill for the actual amount of time spent providing the service (face-to-face and administrative) to the client. Do not bill in blocks of time (e.g., an hour for each individual therapy). Medi-Cal billing is per minute. Please do NOT round up.
- The documentation time that should be included in the total time billed for the service should reflect the actual amount of time spent documenting the service, up to a maximum of 15 minutes. As noted below, documentation time should not be included for late entry notes.
- Timeliness of Service Documentation. Each Service contact is documented in a progress note and documentation must be finalized in a timely manner per the following guidelines.
- A progress note is completed for each service contact. (Except for Crisis Stabilization Unit (CSU) and Crisis Residential services which have daily note requirements).
- For group notes billing, staff must detail the purpose of the group and individualize the note for each client in the group which documents how the client participated in and benefited from the group as well as their individual response to the interventions provided during the group.
- Every effort should be made to complete progress notes on the same day as the session.
- Individual and Group Notes must be finalized within 72 hours or 3 business days from the date of the delivery of the service, except as follows:
- Notes requiring co-signatures must be submitted to a supervisor within 3 business days for review and authorized by the supervisor within 10 business days from the date of service. Upon authorization, the staff requiring co-signature must then finalize the note so that the service can be claimed. If the supervisor is not available, the providing staff must coordinate with the program director or other designated supervisors for reviewing notes and other clinical documents for co-signature.
- If notes are not finalized within 3 (or 10) days, the clinician must write “late entry” in the “Notes” section of the progress note. It should be documented at the beginning of the “S” portion of the formatted note (SIRP). Late entry services should not include documentation time when claiming.
- Documentation must be readable and legible. Ensure that the spell check function is turned on. In Clinician’s Gateway, the “spell check function” button is located near the bottom of page. Always spell check prior to finalizing a document.
- The use of abbreviations in clinical documentation must be consistent with approved BHRS abbreviations. (See Appendix F for a list of approved abbreviations.)
- Restriction of Client Information: APS/CPS Reports, Incident Reports, Unusual Occurrence Forms, Grievances, Notice of Adverse Benefit Determination (NOABD), Utilization Review Committee recommendations or forms and audit worksheets should never be scanned into the electronic health record, or filed within the paper record or billed. Questions regarding other forms (not already listed) and their inclusion into the medical record should be directed to QA/QM staff.
- Confidentiality: Do not write another client’s name in client’s chart. If another client must be identified in the record do not identify that individual as a behavioral health client unless necessary. Names of family members/support persons should be recorded only when needed to complete intake registration and financial documents. Otherwise, refer to the relationship - mother, husband, friend, but do not use names. May use first name or initials of another person when needed for clarification.
- Copy and Paste: Do not copy and paste notes into a client’s medical record. Each note needs to be specific to the service provided. If using a CG template that brings forward text from the previous note, the narrative must be changed to reflect the current service being documented. Progress notes that are submitted which appear to be worded exactly like, or too similar to, previous entries may be assumed to be pasted, i.e., containing inaccurate, outdated, or false information, therefore claiming associated with these notes could be considered fraudulent.
For example: The previous Authorization Period was 1/19/20 20 – 1/18/20 21. The annual Client Plan was completed/finalized on 1/10/20 21. The Service Authorization Period will be 1/1 9 /20 21 – 1/ 18 /202 2. If the Client Plan was renewed/finalized after 1/18/20 21 , the Service Authorization period will shift and begin on the date the Renewed Client Plan was finalized. So, using the Authorization Period from the previous example, the annual Client Plan was Renewed/Finalized on 1/30/20 21. The new Service Authorization period would be 1/30/20 21 – 1/29/202 2. Any service provided during the “gap” (between 1/18/20 21 – 1/29/20 21 ) will not be covered by a Client Plan. (See lockout section for exceptions.) 2.4. TIMEFRAMES FOR SUBMISSION OF DOCUMENTATION FOR SERVICE AUTHORIZATION As previously stated, staff must open an episode prior to providing a service. Additional documentation must be submitted within 60 days of opening if services are to continue. (See also Appendix G.) Required forms prior to Onset of Services or at first contact:
- Admission and Discharge
- Client Profile Form
- Consent to Treatment
- Financial Responsibility Form (UMDAP - Uniform Method of Determining the Ability to Pay)
- Notice of Privacy Practices
- Advance Healthcare Directive Information
- Authorization to Exchange Protected Health Information (HIPAA Form 03-01)
- Behavior Checklists (for Children under 18)
- Family History Form (for Adult clients, if applicable)
- Consents for Medication (if applicable) The following forms need to be completed within sixty (60) days of an initial opening for both Adult and Children’s System of Care providers or for an episode where the client was closed for services for over 180 days (6 months) and is being re-opened to services.
- Initial Clinical Assessment
- Client Plan o Medical Necessity Tab o Adult/Child Client Plan Tab
- Obtain Signature of Beneficiary (Client Plan Signature Addendum) Note: Some clients may have had episodes of services prior to this admission from providers that were not part of the integrated plan. For example: Access Team, Contracted Network Providers, Mobile Crisis Response Team. Tip: Remember, it’s a best practice to complete the Initial Clinical Assessment within 30 days and submit with the Client Plan. That will avoid authorization gaps due to the time involved in getting co-signatures and sending a Client Plan for authorization
ADDITIONAL TREATMENT TEAM PROVIDERS
When a client is opened to additional treatment teams, the on-coming service provider is responsible for ensuring the timely submission of Intake and Annual Forms for service authorization. Prior to Onset of Services or at first contact:
- Admission and Discharge form
- Client Profile Form
- Consent to Treatment
- Financial Responsibility Form (UMDAP - Uniform Method of Determining the Ability to Pay)
- Notice of Privacy Practices
- Advance Healthcare Directive Information
- Authorization to Exchange Protected Health Information (HIPAA Form 03-01)
- Behavior Checklists (for Children under 18)
- Family History Form (for Adult clients, if applicable)
- Consents for Medication (if applicable) The on-coming provider must complete the following within 30 days of the opening of the episode:
- Client Plan o Adult/Child Client Plan Tab
- Obtain Signature of Beneficiary (Client Plan Signature form/Client Plan Signature Form)
- Medication Consents (if applicable) The service authorization period remains fixed and is based on the finalized date of the initial Client Plan. ANNUAL RENEWAL OF SERVICES On an annual basis, a reevaluation of the individual’s status and needs must be completed in order to obtain continued authorization for services. It is good practice to review the limits of confidentiality and risks and benefits with the individual as often as clinically relevant. When the service authorization period ends, the primary author is responsible for the completion of the Client Plan and Reassessment. The primary author is responsible for collaboration and monitors goals/objectives amongst the various service providers so that the Client Plan remains relevant to the client’s current behavioral health needs. The following will determine who the primary author is:
- All clients open to our system of care should have a County Case Manager/Therapist who is the primary author for overseeing the renewal of the Client Plan and any required annual documents at the time of the annual renewal period.
- If client is open to Medication Only, the medication practitioner will be primary author.
- If client is not open to a County team, then the primary Organizational/Network provider becomes the primary author. The Primary Author is responsible for the completion of the following forms, which may be completed within the 30 days prior to the end of the Service Authorization period:
- Annual Clinical Reassessment
- Annual Client Plan:
THE FLOW OF CLINICAL INFORMATION As each client begins services with BHRS there is a flow of information designed to support staff in providing services that help the clients meet their recovery goals.
- The Clinical Assessment is the first step toward establishing Medical Necessity and the start of services.
- The Assessment supports staff in developing a Clinical Formulation that informs the diagnostic process.
- The Client Plan creates a framework for the services we provide. Together with clients we develop goals and planned interventions that support the clients in their recovery.
- Each Service provided links back to an issue identified on a Client Plan through the Assessment. Throughout the course of treatment, from Assessment to discharge, all services are based on Medical Necessity. Meaning, every service provided to the client/family is medically necessary to support the client/family in their path to recovery. 3.1. ASSESSMENT The Assessment is more than an information gathering process. The Assessment is the first step towards building a trusting and therapeutic relationship between client and service provider. It is also an important beginning to understand and appreciate who the client is and the interrelationship between the client’s symptoms/behaviors and the client as a whole person.
Assessment
- Clinical Formulation
- Client Plan
- Services Medical Necessity Chapter 3. ESTABLISHMENT OF MEDICAL NECESSITY
The initial assessment is an important first step to get a clear account of the current problems. Providers have a responsibility to fully understand the individual and family, their strengths, abilities, and past successes, along with their hopes, dreams, needs, and problems in seeking help. Attending to the issues of culture in the process of the assessment is critically important. The provider must understand how culture and social context shape an individual’s and family’s behavioral health symptoms, presentation, meaning and coping styles along with attitudes towards seeking help, stigma and the willingness to trust. The assessment can be completed in one contact or over the course of several contacts. The assessment must contain:
- Presenting problems and relevant conditions affecting physical and mental health status (e.g. living situation, daily activities, and social support, cultural and linguistic factors and history of trauma or exposure to trauma).
- Mental health history, previous treatments dates, providers, therapeutic interventions and responses, sources of clinical data, relevant family information, lab tests, and consultation reports.
- Physical health conditions reported by the client are prominently identified and updated.
- Name and contact information for primary care physician.
- Medications, dosages, dates of initial prescription and refills, and informed consent(s).
- Past and present use of tobacco, alcohol, and caffeine, as well as illicit, prescribed, and over-the-counter drugs.
- Client strengths in achieving goals.
- Special status situations and risks to client or others.
- Allergies and adverse reactions, or lack of allergies/sensitivities.
- Mental Status Examination (included on the psychosocial Assessment).
- Diagnosis consistent with the presenting problems, history, mental status examination and/or other clinical data. In cases where services are provided due to a suspected mental health disorder that has not yet been diagnosed or due to significant trauma (for clients under 21), options are available in the CMS approved ICD-10 diagnosis code list. These include codes for “Other specified” and “Unspecified” disorders,” or “Factors influencing health status and contact with health services” (Z codes).
- For children and adolescents, prenatal events, and complete developmental history.
- All required elements in the assessment must be completed. Do not leave any item blank. If unable to answer, please put N/A for an item.
- Additional clarifying formulation information, as needed. It is important to note the name of the Primary Care Physician (PCP) on the assessment. The Clinical Assessment/Reassessment found in CG is compliant with all State and Federal Regulations. However, the service provider (author) must ensure that all sections of the Clinical Assessment/Reassessment are filled out. Use the “leading questions” located next to each section header. Do not leave sections blank as this may cause a mandated section to remain unassessed and may lead to disallowances. Answer the “leading questions” ➔
3.3. COMPONENTS OF MEDICAL NECESSITY DHCS has issued the following descriptions of medical necessity access criteria for Specialty Mental Health Services (SMHS) 3.3.1. Criteria for Beneficiaries 21+ Beneficiary meets both of the following criteria, (1) and (2) below: (1) The beneficiary has one or both of the following: a. •Significant impairment, where impairment is defined as distress, disability, or dysfunction in social, occupational, or other important activities. b. A reasonable probability of significant deterioration in an important area of life functioning AND the condition is due to either of the following: a. •A diagnosed mental health disorder, according to the criteria of the DSM and the ICD. Or b. •A suspected mental disorder not yet diagnosed. 3.3.2. Access Assurances for Beneficiaries under 21 For enrolled beneficiaries under 21 years of age, BHRS shall provide all medically necessary specialty mental health services required pursuant to Section 1396d(r) of Title 42 of the United States Code. Covered specialty mental health services shall be provided to enrolled beneficiaries who meet either of the following criteria, (1) or (2) (1) The beneficiary has a condition placing them at high risk for a mental health disorder due to experience of trauma evidenced by any of the following: scoring in the high-risk range under a trauma screening tool approved by DHCS, involvement in the child welfare system, juvenile justice involvement, or experiencing homelessness. Or (2) The beneficiary meets both of the following requirements in a) and b), below a) The beneficiary has at least one of the following: i. A significant impairment ii. A reasonable probability of significant deterioration in an important area of life functioning iii. A reasonable probability of not progressing developmentally as appropriate iv. A need for specialty mental health services, regardless of presence of impairment, that are not included within the mental health benefits that a Medi-Cal managed care plan is required to provide And
b) The beneficiary’s condition as described above is due to one of the following : i. A diagnosed mental health disorder, according to the criteria of the current editions of the Diagnostic and Statistical Manual of Mental Disorders and the International Statistical Classification of Diseases and Related Health Problems ii. A suspected mental health disorder that has not yet been diagnosed iii. Significant trauma placing the beneficiary at risk of a future mental health condition, based on the assessment of a licensed mental health professional. If a beneficiary under age 21 meets the criteria as described in (1) above, the beneficiary meets criteria for SMHS; it is not necessary to establish that the beneficiary also meets the criteria in (2) above. Per Welfare and Institutions Code section 14184.402(f)(1)(A), a mental health diagnosis is not a prerequisite for access to covered SMHS. This does not eliminate the requirement that all Medi-Cal claims, including SMHS claims, include a CMS approved ICD-10 diagnosis code. 9 In cases where services are provided due to a suspected mental health disorder that has not yet been diagnosed or due to trauma as noted above, options are available in the CMS approved ICD-10 diagnosis code list. For example, these include codes for “Other specified” and “Unspecified” disorders,” or “Factors influencing health status and contact with health services” (i.e., Z codes). Definitions: Involvement in Child Welfare The beneficiary has an open child welfare services case, which means that the child welfare agency has opened a child welfare or prevention services case with the family to monitor and provide services. A child has an open child welfare or prevention services case if: a) the child is in foster care or in out of home care, including both court-ordered and by voluntary agreement; or b) the child has a family maintenance and/or prevention services case (pre-placement or post-reunification), including both court-ordered and by voluntary agreement. A child can have involvement in child welfare whether the child remains in the home or is placed out of the home. Involvement in child welfare also includes a child whose adoption occurred through the child welfare system. Definitions: Homelessness The federal Department of Housing and Urban Development’s most recent definition of homelessness includes four categories:
- Literally homeless
- Imminent risk of homelessness
- Homeless under other Federal statutes
- Fleeing/attempting to flee domestic violence Definitions: Juvenile Justice Involvement The beneficiary: has ever been detained or committed to a juvenile justice facility, or is currently under supervision by the juvenile delinquency court and/or a juvenile probation agency Beneficiaries who have ever been in custody and held involuntarily through operation of law enforcement authorities in a juvenile justice facility, including youth correctional institutions, juvenile detention facilities, juvenile justice centers, and other settings such as boot camps, ranches, and forestry/conservation camps, are included in the “juvenile justice involvement” definition.
4.1. CLIENT PLAN Key points of Client Plan documentation
- Provides the focus of treatment
- Contains Client’s Goals, including their hopes and dreams
- Highlights client’s/family’s strengths to achieve their goals.
- Lists Objective(s) - that which is to be accomplished by the treatment
- Needs to be “specific, observable and/or measurable”.
- Must focus on impairments.
- Identifies Intervention(s) – how the service provider intends to address the impairment (not just the modality).
- Include the frequency and duration of the intervention
- Needs to be consistent with the client’s goals and clinical objectives
- Is completed prior to the delivery of planned services and within 60 days of the start of service, and no less than annually thereafter.
- Client signature documents their participation in the development of the Client Plan.
- Clients are offered a copy of the plan and whether they accept or decline is documented. Marin Behavioral Health and Recovery Services (BHRS) embraces the “One Client Plan” model for the delivery of services. This means that all programs, whether from BHRS programs or community partners, create treatment objectives for their specific program with the client/family in a Client Plan. If more than one program or provider is involved, these program specific objectives are coordinated into one overall Client Plan. This model helps the client understand who is providing what services and more specifically, what the expectations are for each provider. The Client Plan, co-created by the client/family and the provider, outlines the goals, objectives, interventions and timeframes. The Plan must substantiate ongoing medical necessity by focusing on diminishing the impairment(s) and/or the prevention of deterioration that has been identified through the assessment process and the clinical formulation. The impairment(s) and/or deterioration to be addressed must be consistent with the diagnosis that is the focus of treatment. Program objectives should be consistent with the client’s/family’s goals as well. Strength- based and recovery oriented treatment planning is strongly encouraged. Translating Client Goals into specific, observable/measurable objectives requires considerable skill. Usually what is involved is uncovering concrete issues, behaviors, or barriers that are preventing the client from accomplishing their goal. Following this is a discussion to frame the issue/barrier in a way that is acceptable to the client but is also meaningful in terms of focusing services. These discussions can all be claimed as Plan Development. An ideal objective is one that that meets both the client’s needs in working towards the goal and is specific and measurable enough to be able to chart progress. The client’s participation and understanding of all elements of the plan is essential for successful outcomes and is required by state regulations. The only exception is when a person has a legal status that removes individual decision-making power, e.g., an LPS Conservatorship. Chapter 4. TREATMENT PLANNING W&I Code Sec. 5600.2. (a) (2) states (Persons with mental disabilities) “Are the central and deciding figure, except where specifically limited by law, in all planning for treatment and rehabilitation based on their individual needs. Planning should also include family members and friends as a source of information and support.”
4.1.1. CLIENT PARTICIPATION AND SIGNATURES:
- Client participation is documented by obtaining the signature of the client/parent/guardian on the “Client Plan Signature Form” or by electronic signature on the plan. The following signatures should be present on the “Client Plan Signature Form”: - Client or Legal Responsible Party (if the client is under the age of 12 or is a conserved adult). A minor can legally sign their Plan if he/she is at least 12 years old. It is encouraged that a parent/legal responsible party, i.e., CFS worker, conservator, etc. signature be obtained whenever possible. (See also section 8.1, Minor Consent.) - Program staff member completing the Plan. - All BHRS county Client Plans must be authorized by program supervisor. - All contractor Client Plans must be authorized by county program supervisor or designated contractor supervisor. - The authorization signature will also act as a co-signature for staff that need co-signatures on documentation.
- If a client or parent/guardian refuses to sign or is unavailable to sign, the clinician completes the box on the client plan documenting the reason that the parent/guardian signature was not obtained in a timely manner. Continue to attempt to get a signature and document these attempts in progress notes. The following signature related activities should be documented. - Phone contact(s) or letters (keep a copy in the chart under correspondence) - Discussions between client/family and provider when the provider discusses the Client Plan goals over the phone and the parent/guardian accepts/agrees to the Client Plan goals. - When a copy of the Client Plan is mailed to parent/guardian for a signature along with any follow-up until the sign copy is received and filed.
- In addition to the client’s signature as evidence of the client’s participation on the Client Plan, the service provider should document and date that they offered of a copy of the Client Plan to the client/guardian. This field is required. 4.1.2. TIMELINESS OF CLIENT PLANS The Initial Client Plan must be completed within sixty (60) days of an admission for both Adult and Children’s System of Care providers or for an episode in which the client was closed for services for over 180 days (6 months) and is being re-opened to services: Due to the time involved in sending a Client Plan for authorization, getting co-signatures and possibly other providers’ contribution of objectives and interventions, it is strongly suggested that the Client Plan, along with the Initial Clinical Assessment, be completed and submitted within 30 days of opening. As previously stated, documentation of the client’s participation (client’s signature) is mandatory and must be entered into the record within the same time frames. Client Plans must be reviewed and renewed on an annual basis. For example, the “established service authorization period” is 2/15/ 21 to 2/14/ 22 , the Annual Client Plan must be finalized and signatures obtained by 2/1 5 / 21 so that there is no break in service authorization. If there is a lapse between expiration and renewal dates, then those services covered by the plan (“planned services”) occurring during the lapse are subject to disallowance. It is important to avoid lapses in renewals of annual Client Plans. See also Lockouts and Limitations.