







































































Study with the several resources on Docsity

Earn points by helping other students or get them with a premium plan


Prepare for your exams
Study with the several resources on Docsity

Earn points to download
Earn points by helping other students or get them with a premium plan
Community
Ask the community for help and clear up your study doubts
Discover the best universities in your country according to Docsity users
Free resources
Download our free guides on studying techniques, anxiety management strategies, and thesis advice from Docsity tutors
The purpose of this manual is to provide billing information regarding services provided by 29-I. Licensed Health Facilities and administered by the New ...
Typology: Study notes
1 / 91

This page cannot be seen from the preview
Don't miss anything!






































































The purpose of this manual is to provide billing information regarding services provided by 29-I Licensed Health Facilities and administered by the New York State Department of Health (NYS DOH) and Office of Children and Family Services (OCFS). This manual applies to services covered by both Medicaid Managed Care (MMC) and Medicaid fee-for-service (FFS) and outlines the claiming requirements necessary to ensure proper claim submission for services delivered by a 29-I Health Facility. This manual is intended for use by both Medicaid Managed Care Plans (MMCP) and 29-I Health Facilities.
This manual provides billing guidance only. It does not supersede applicable regulatory requirements or procedures for admission to a program, record keeping, service documentation, initial and on-going treatment planning, and reviews, etc. The contents of this manual may be subject to change as required.
Voluntary Foster Care Agencies (VFCAs) that have not obtained 29-I licensure are NOT authorized to provide and/or bill for health care services outlined in this guidance. All VFCAs that are licensed as 29-I Health Facilities will have a NYS DOH issued license indicating authorization to bill for Core Limited Health-Related Services and Other Limited Health-Related Services. This manual does NOT provide guidance regarding Maximum State Aid Rates (MSAR) payments. MSAR information and guidance can be found at https://ocfs.ny.gov/main/Rates/FosterCare/Manual/SOP-ProgramManual.pdf.
VFCAs serving principally as facilities for the care of and/or boarding out of children shall be subject to the provisions of Article 29-I of the Public Health Law (PHL) and applicable state and federal laws, rules, and regulations. While 29-I licensure is optional, VFCAs are required to obtain and maintain 29-I licensure to bill eMedNY and MMCPs for the services listed in this document.
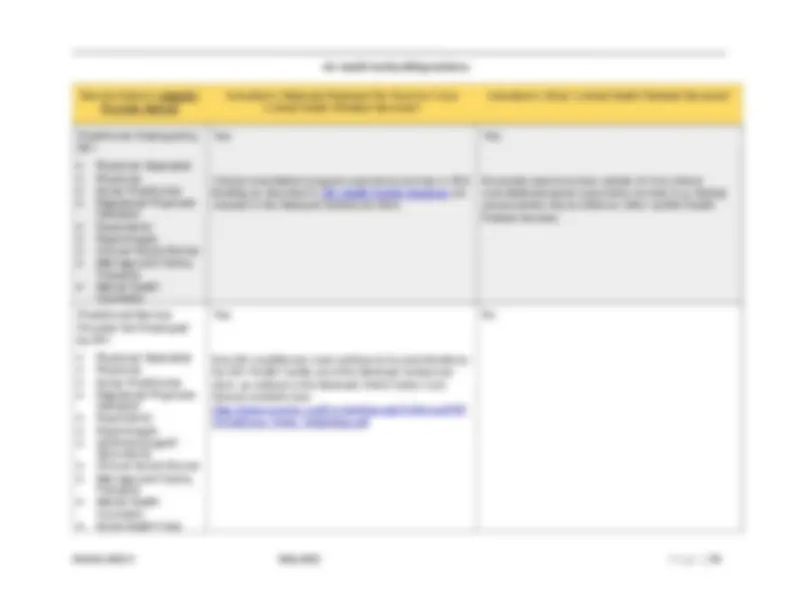
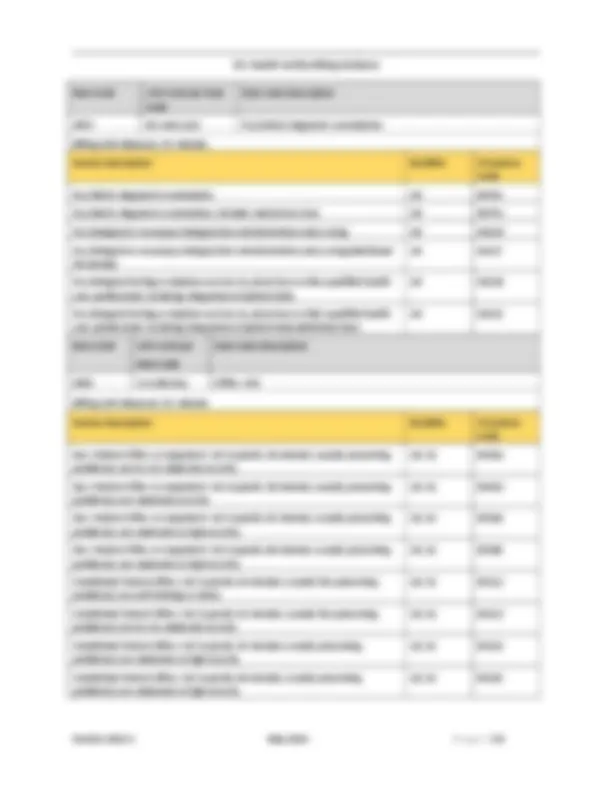
There are two categories of services that can be provided within 29-I Health Facilities: Core Limited Health-Related Services (Mandatory) and Other Limited Health-Related Services (Optional). 29-I Health Facilities must provide all Core Limited Health-Related Services. The Core Limited Health-Related Services as described in this schedule, and the associated billing, are available only to children/youth in the care of a 29-I Health Facility.
Pursuant to Article 29-I of Section 1 of the Public Health Law (PHL), VFCAs must be licensed for the provision of Core Limited Health-Related Services and Other Limited Health-Related
Services as described above in order to contract with and bill MMCPs and comply with Corporate Practice of Medicine standards.
To become licensed as a 29-I Health Facility, the providers must submit an application to OCFS and DOH, which indicates the location and describes the physical environment where each of the Core Limited Health-Related Services and any Other Limited Health-Related Services will be provided. In addition, the application must demonstrate compliance with all required rules and regulations. Additional information regarding Core Limited Health-Related Services, Other Limited Health-Related Services, and 29-I licensing requirements can be found at https://www.health.ny.gov/health_care/medicaid/redesign/behavioral_health/children/vol_fo ster_trans.htm.
2.2 MEDICAID-ENROLLED PROVIDER
All eligible health care providers are required to enroll in Medicaid in order to receive reimbursement for delivering a Medicaid service.
29-I Health Facilities must be enrolled with category of service code 0121 to bill for Core Limited Health-Related Services, and category of service code 0268 to bill for Other Limited Health-Related Services.
Information on how to become a Medicaid provider is available on the eMedNY website: https://www.emedny.org.
2.3 MEDICAID MANAGED CARE CONTRACTING
To be paid for services delivered to a child/youth enrolled in a Medicaid Managed Care Plan, a provider must be contracted and credentialed with that MMCP for the service rendered (i.e. in the MMCP’s network). Plans must enter into Single Case Agreements (SCAs), if needed, to facilitate payment to a 29-I Health Facility who has not contracted with the MMCP and will deliver services to a child/youth. More information on Medicaid Managed Care contracting can be found in the Transition of Children Placed in Foster Care and NYS Public Health Law Article 29-I Health Facility Services into Medicaid Managed Care
2.4 PROVIDERS DESIGNATED TO DELIVER CFTSS AND CHILDREN’S HCBS SERVICES
29-I Health Facilities may provide Children and Family Treatment and Support Services (CFTSS) and Children’s Home and Community Based Services (HCBS) as part of their Other Limited Health-Related Services. 29-I Health Facilities who wish to provide CFTSS and HCBS are required to receive the appropriate designation(s) from the State.
Additional information can be found on the NYS Children’s Behavioral Health System Transformation webpages:
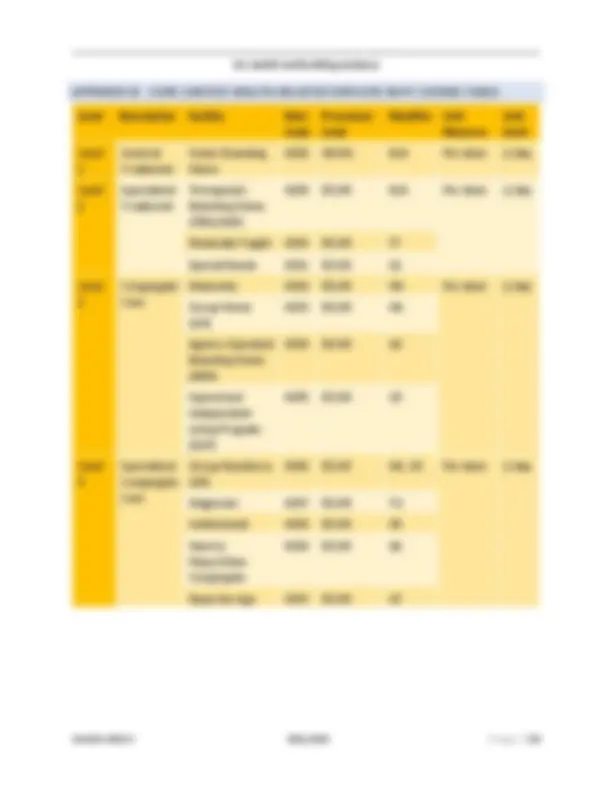
The Medicaid residual per diem rate reimburses 29-I Health Facilities for Core Limited Health- Related Services and is associated with the 29-I facility type (see Table 1: 29-I Health Facility Types ) and indicated on the Article 29-I License. All 29-I Health Facilities are required to provide the Core Limited Health-Related Services to all children residing in the facility. Services are standardized across each facility type and are reimbursed based on a standardized Medicaid residual per diem rate schedule. Core Limited Health-Related Services (Medicaid per diem) rates can be found at https://www.health.ny.gov/health_care/medicaid/redesign/behavioral_health/children/vol_fo ster_trans.htm
Core Limited Health-Related Services are reimbursed with a Medicaid residual per diem rate paid to 29-I Health Facilities on a per child/per day basis to cover the costs of these services. For children/youth not enrolled in a plan, providers must bill Medicaid Fee-for service (FFS) via eMedNY. For members who are enrolled in a managed care plan, providers must bill the MMCP. The MMCP will bill the State for the per diem as pass through for the four-year transition period. At the end of the transition period, the State will reassess progress of the implementation and determine if transitional requirements should be extended.
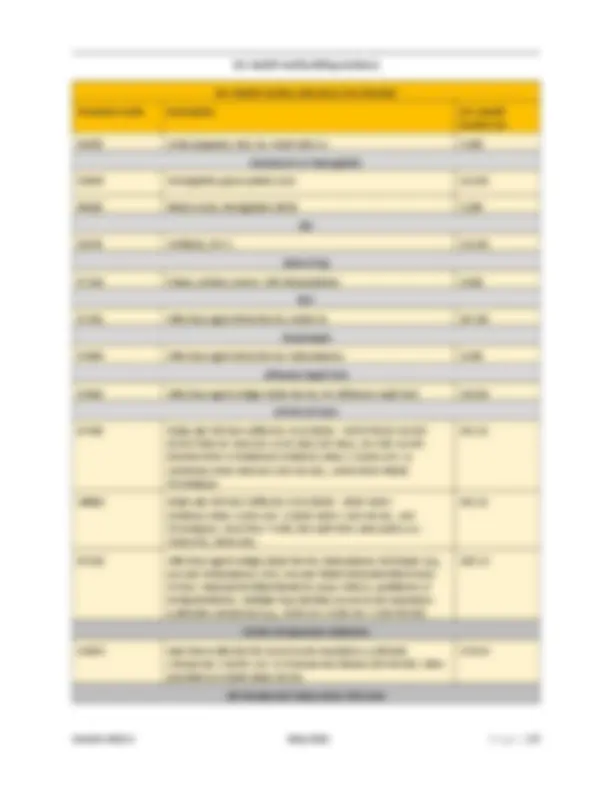
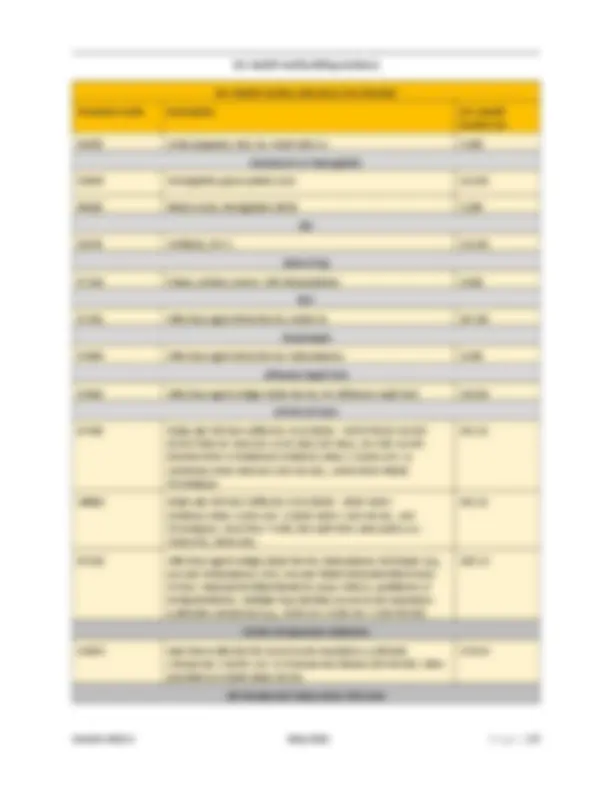
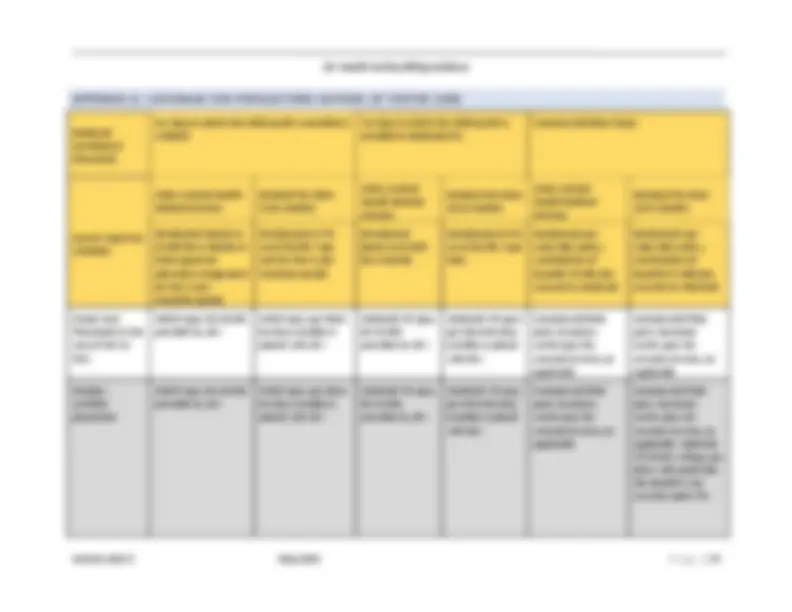
Article 29-I of the PHL indicates which level(s) of care are provided by each 29-I Health Facility. 29-I Health Facilities are categorized by the level of care provided, as outlined in Table 1: 29-I Health Facility Types. Core Limited Health-Related Services (Medicaid residual per diem) rates differ based on both the level of care and the facility type the 29-I Health Facility is operating, with one rate assigned to each of the 13 facility types. Since a 29-I Health Facility may operate more than one facility type in one or more levels of care, it may be necessary for a 29-I Health Facility to bill several different Core Limited Health-Related Services (Medicaid per diem) rates, depending on how many facility types that 29-I Health Facility operates. The Core Limited Health-Related Services (Medicaid per diem) rate billed must correspond to the rate for the facility type the individual child/youth is residing in. However, only one Core Limited Health- Related Services (Medicaid per diem) rate per day for each individual child/youth can be billed. The Medicaid residual per diem rate is paid for the duration of the child’s stay in the 29-I Health Facility; there are no annual or monthly limits applied to the per diem rate. There are four (4) levels of care, which are identified in the table below:
Level Description Facility Type Level 1 General Treatment (^) • Foster Boarding Home Level 2 Specialized Treatment • Therapeutic Boarding Home (TBH)/AIDS
29-I Health Facilities are reimbursed to provide the Core Limited Health-Related Services under the Article 29-I licensure through the Medicaid residual per diem, which are paid by MMCPs to the 29-I Health Facility (or Fee-For-Service Medicaid for those children not enrolled in Managed Care).
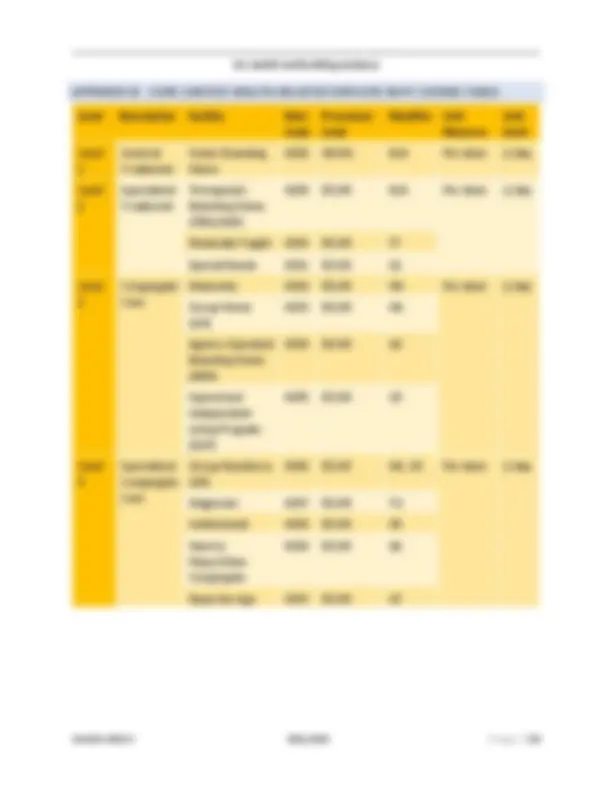
Refer to Appendix B for a list of the 13 Core Limited Health-Related Services rate codes that correspond to the level and facility type.
3.3 CORE LIMITED HEALTH-RELATED SERVICES RATES FOR STEP DOWN AGENCIES
Transitional rates will be updated yearly beginning July 1, 2021 through July 1, 2024. On July 1, 2024, all 29-I Health Facilities will be reimbursed the standard rate schedule based on facility type. For 29-I Health Facilities that are receiving a transitional rate for Core Limited Health- Related Services, rates will be specific to the facility type that is transitioning with a unique agency-based rate.
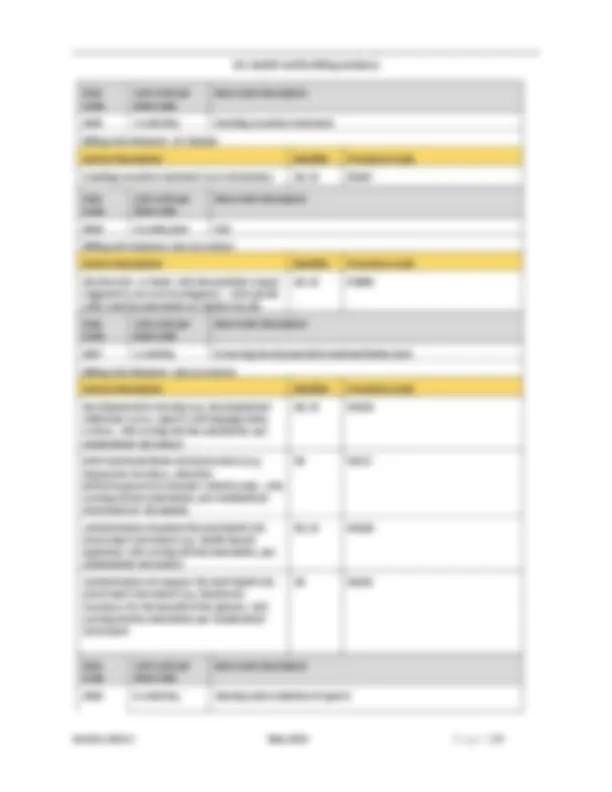
3.4 OTHER LIMITED HEALTH-RELATED SERVICES (OPTIONAL SERVICES A 29-I HEALTH FACILITY MAY PROVIDE)
The Other Limited Health-Related Services that can be provided by a 29-I Health Facility to meet a child/youth’s individualized treatment goals and health needs are listed below. All Other Limited Health-Related Services that a 29-I Health Facility provides must be included in the 29-I
Other Limited Health-Related Services do not include the following services, which should be provided by Medicaid participating providers (i.e. essential community providers) and billed directly by these providers to MMCPs/Medicaid FFS:
Other Limited Health-Related Services do not include nursing services, skill building activities (provided by LBHPs as described Article 29-I VFCA Health Facilities License Guidelines and any subsequent updates), and Medicaid treatment planning and discharge planning, including medical escorts and any clinical consultation/supervision services and tasks associated with the Managed Care Liaison/administrator in 29-I Health Facilities. These services are included in the Preventive or Rehabilitative Residential supports of the mandatory Core Limited Health-Related Services.
Other Limited Health-Related Services may be provided to children/youth in the care of any 29-I Health Facility, including children/youth in foster care, children/youth placed in a 29-I Health Facility by Committee on Special Education (CSE), babies residing with their parent who are placed in a 29-I Health Facility and in foster care, pre-dispositional placed youth, and children/youth in foster care placed in a setting certified by the Local Department of Social Services (LDSS).
Children/youth who are discharged from a 29-I Health Facility may continue to receive Other Limited Health-Related Services from any 29-I Health Facility up to one-year post discharge. These services may continue beyond the one-year post discharge date, if any of the following apply:
o the Enrollee has been placed in the care of the 29-I Health Facility and has been in receipt of Other Limited Health-Related Services prior to their 21 st^ birthday, and the Enrollee has not yet safely transferred to another placement or living arrangement: and o the Enrollee and/or their authorized representative is compliant with a safe discharge plan; and o the 29-I Health Facility continues to work collaboratively with the MMCP to explore options for the Enrollee’s safe discharge, including compliance with court ordered services, if applicable.
29-I Health Facilities will be reimbursed for Core and Other Limited Health-Related Services by MMCPs for children enrolled in Medicaid Managed Care or by Fee-For-Service Medicaid for children who are not enrolled in Medicaid Managed Care.
3.7 AGENCIES WITHOUT A 29-I LICENSURE
Agencies that do not obtain Article 29-I Licensure are not authorized to receive a Medicaid per diem to provide Core Limited Health-Related Services.
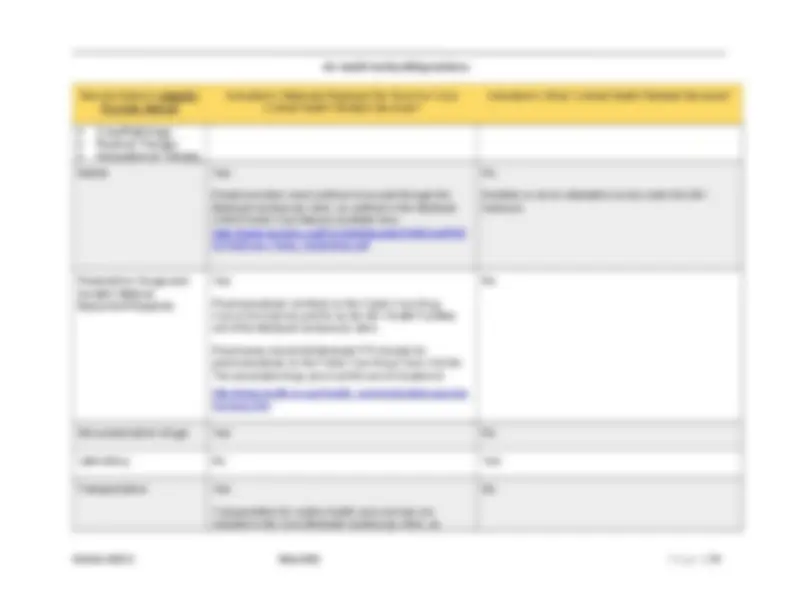
3.8 CORE LIMITED HEALTH-RELATED SERVICES REGIONS
Core Limited Health-Related Services are not subject to regional reimbursement differences, as the Medicaid per diem was calculated as a statewide Medicaid rate. The Medicaid per diem is assigned to 29-I Health Facilities based on the facility types they are authorized to operate under an Article 29-I License.
3.9 OTHER LIMITED HEALTH-RELATED SERVICES REGIONS
The regions as defined by the Department of Health and assigned to providers based upon the geographic location of the provider’s headquarters are defined as follows:
3.10 MEDICAID MANAGED CARE PLAN PAYMENTS
MMCPs must reimburse the NYS Medicaid FFS rates for Core Limited Health-Related Services for the four-year transition period from July 1, 2021 through June 30, 2025. MMCPs must reimburse Other Limited Health-Related Services for the four-year transition period at the Medicaid FFS fee schedule (where available), unless alternative arrangements have been made between plans and providers and have been approved by DOH and OCFS (e.g., Value-Based Payment arrangements). MMCPs should submit passthrough payments for Core Limited Health Related Services to the State within 30 days of claim payment, and no later than 180 days from date of service. For pass through claims that are submitted more than 90 days after the date of service, plans should use Delay Reason Code “03” to avoid claims rejecting due to untimely filing. Please note, while use of Delay Reason Code 03 typically requires claim submission on paper, the State has implemented a system edit to allow for managed care plans to 29-I Core Limited Health Related Services claims electronically when using Delay Reason Code 03.
At the end of the transition period, the State will reassess progress of the implementation and determine if transitional requirements should be extended.
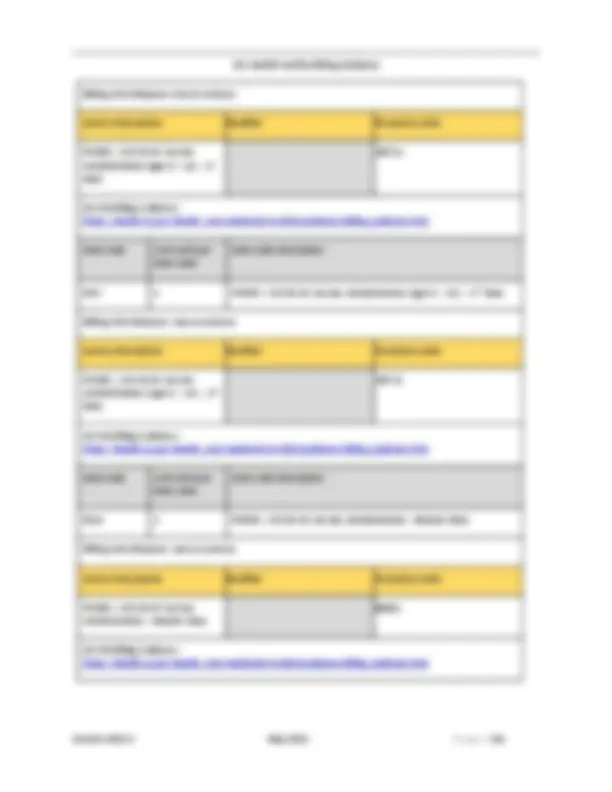
Reimbursement for Interpreter Services for children/youth receiving care by a 29-I Health Facility is available for services provided during a medically necessary encounter for the following Other Limited Health Related Service rate codes: 4588, 4589, 4590, 4591, 4592, 4593, 4594, 4595, 4596, 4597, 4598.
The need for medical language interpreter services must be documented in the medical record and must be provided during an encounter. The 29-I Health Facility is responsible for developing a business relationship with one or more agencies that can provide trained, competent interpreters in the needed language(s). Interpreter services provided by the 29-I Health Facility staff are not eligible for reimbursement. These interpreter services may be provided in person by an interpreter or by telephone with a translation service. The interpreter must demonstrate competency and skills in medical interpretation techniques, ethics, and terminology. It is recommended, but not required, that such individuals be recognized by the National Board of Certification for Medical Interpreters (NBCMI). The provider must document the encounter in the child/youth’s medical record and include the location, type of interpretation provided, name of interpreter, and agency. Interpretation services also includes sign language for individuals who are deaf or hearing impaired.
Rate Code Procedure code Modifier Max Units Description
4673 T1013 2 units/encounter
In person interpreter services
4673 T1013 GQ 2 units/encounter
Telephone interpreter services
One Unit: Includes a minimum of eight and up to 22 minutes of medical language interpreter services.
Two Units: Includes 23 or more minutes of medical language interpreter services.
The time billed for interpretation services cannot exceed the length of time of the encounter. Claims must be submitted by the 29-I Health Facility providing the service. The rate of payment will be set at $11.00 for one unit of service up to a maximum of two billable units of service per patient per encounter. If the child/youth is seen for more than one encounter in a day, interpretation services may be billed for up to two units per encounter. Each claim must include rate code 4673 and Healthcare Common Procedure Coding System (HCPCS) procedure code
o the types of providers that can deliver the services; o the specific nature of the services; and o the programmatic framework within which the services can be delivered, including supervision requirements.
Additionally, the services must be those that are covered by New York State Medicaid.
4.2 MEMBER ENROLLMENT STATUS
Before delivering services to an individual, providers should always check ePaces to verify the individual’s Medicaid enrollment status and MMCP enrollment status. Providers should verify individual Medicaid and MMCP enrollment through the NYS system. Claims will not be paid if a claim is submitted for an individual who is not enrolled with Medicaid, an individual is not eligible for the service provided, or if the claim was submitted to an incorrect MMCP. Providers should always verify that claims are submitted to the correct MMCP.
Providers may appeal claims that have been denied; providers may contact the MMCP for information on how to appeal claim denials. In certain circumstances, providers may file a complaint or external appeal with State agencies. See also https://www.health.ny.gov/health_care/managed_care/complaints/.
4.3 29-I HEALTH FACILITY MEDICAID FEE-FOR-SERVICE CLAIMING (EMEDNY)
Claims for services delivered to an individual in receipt of fee-for-service Medicaid are submitted by providers to eMedNY. See https://www.emedny.org for training on use of the eMedNY system.
Claim submissions must adhere to the 90-day timely filing rules for Medicaid FFS. See State Medicaid billing guidance available at https://www.emedny.org/info/TimelyBillingInformation_index.aspx.
4.4 GENERAL MEDICAID MANAGED CARE CLAIMING FOR 29-I HEALTH FACILITIES (ALL SERVICES)
MMCPs and providers must adhere to the billing and coding manual requirements of this manual as well as clean claiming rules as outlined in billing tool found here: https://www.health.ny.gov/health_care/medicaid/redesign/behavioral_health/children/vol_fo ster_trans.htm
The MMCP shall support both paper and electronic submission of claims for all claim types. The MMCP shall offer providers an electronic payment option including a web-based claim submission system. MMCPs rely on Current Procedural Terminology (CPT) codes and modifiers when processing claims. Therefore, all MMCPs will require claims to be submitted with the CPT
code and modifier (if applicable) in addition to the State-assigned rate code. Please refer to Appendix B and Appendix C for a complete listing of CPT codes and associated modifiers. Claims must include a National Provider Numbers (NPI) associated with the 29-I Health Facility.
MMCPs will be provided with a complete listing of all existing 29-I Health Facilities and the rate codes they are authorized to bill under, as well as the rate amounts by MMIS provider ID, locator code, and/or NPI and zip+4. Billing requirements depend on the type of service provided.
Providers must adhere to timely filing guidelines as outlined in their contract with the MMCP and per eMedNY guidelines (https://www.emedny.org/info/TimelyBillingInformation_index.aspx). When a clean claim is received by the MMCP, they must adjudicate per prompt pay regulations. If a provider does not have a contract or a Single Case Agreement in place with the MMCP, the claim can be denied. Providers may contact the MMCP for information on how to appeal claim denials. In certain circumstances, providers may file a complaint or external appeal with State agencies. See also https://www.health.ny.gov/health_care/managed_care/complaints/
It is the provider’s responsibility to determine the type of coverage (Medicare, Medicaid, or private insurance) that the member is eligible to receive. Medicaid is the payor of last resort and all Medicare and third-party coverage must be exhausted before payment for 29-I health services by Medicaid.
Acceptable documentation of attempts to secure third party reimbursement as required under 18 NYCRR §540.6, includes documentation of a rejection by third party insurance for a date of service within the previous 12 months of the date of service being billed, or since a change in third party coverage, whichever is later. See the following regulation for more information: https://regs.health.ny.gov/content/section-5406-billing-medical-assistance.
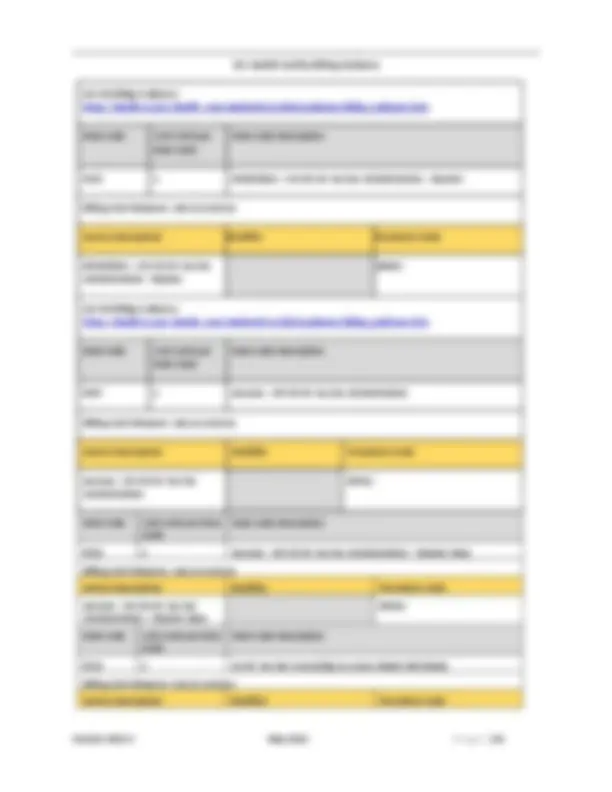
4.5 MEDICAID MANAGED CARE CLAIMING FOR CORE LIMITED HEALTH-RELATED SERVICES
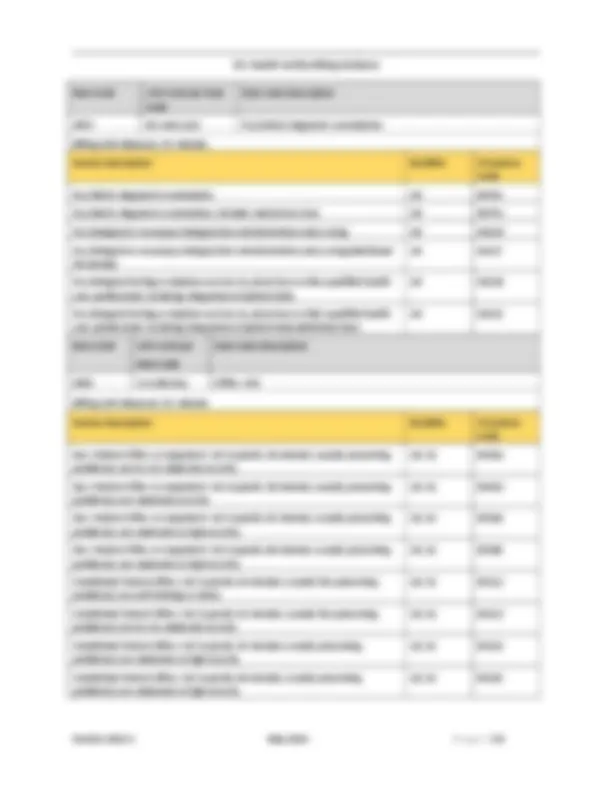
For 837i and UB-04 claims, the 29-I Health Facility will enter the rate code in the header of the claim as a value code. This is done in the value code field by first typing in “24” followed immediately with the appropriate four-digit rate code. This is the standard mechanism used in Medicaid FFS billing.
The 837i (electronic) or UB-04 (paper form) is used to bill for Core Limited Health-Related Every claim must include the following:
General Billing Guidance for Institutional service claims (837i/UB-04) form can be found at
Guidance regarding billing for the use of interpretation services can be found at https://www.health.ny.gov/health_care/medicaid/program/update/2012/oct12mu.pdf.
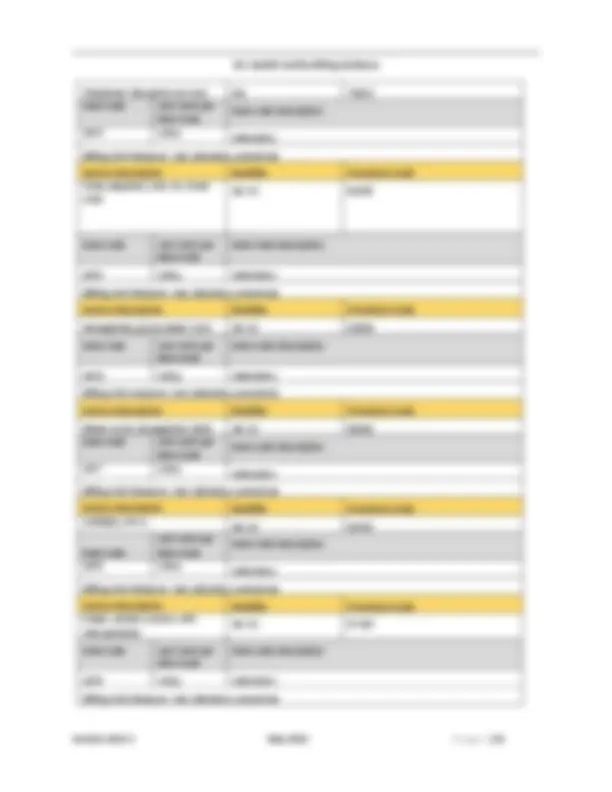
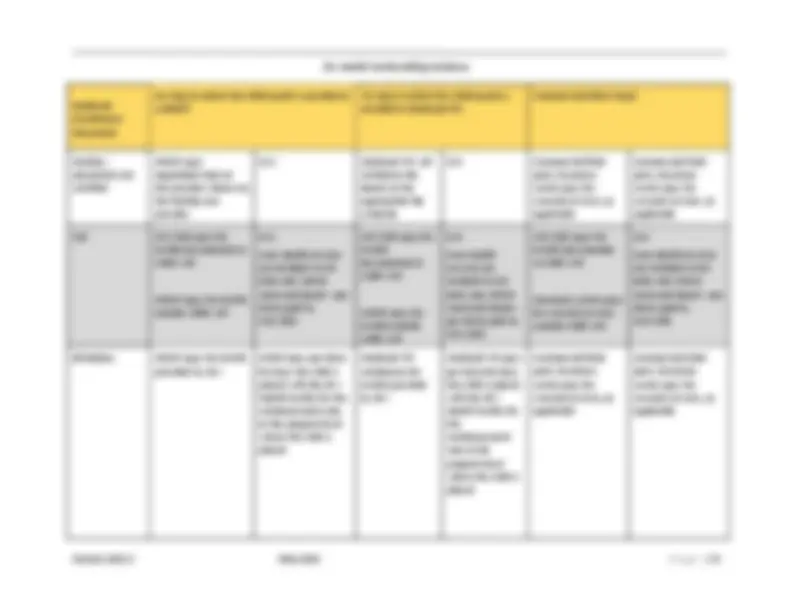
Providers must include the applicable rate code, CPT codes, and modifiers (see Appendix C for billable and non-billable procedure codes). If there are two modifiers needed for one procedure code, both modifiers must be present and do not require a provider to indicate them in the exact same order for every claim for payment to be made.
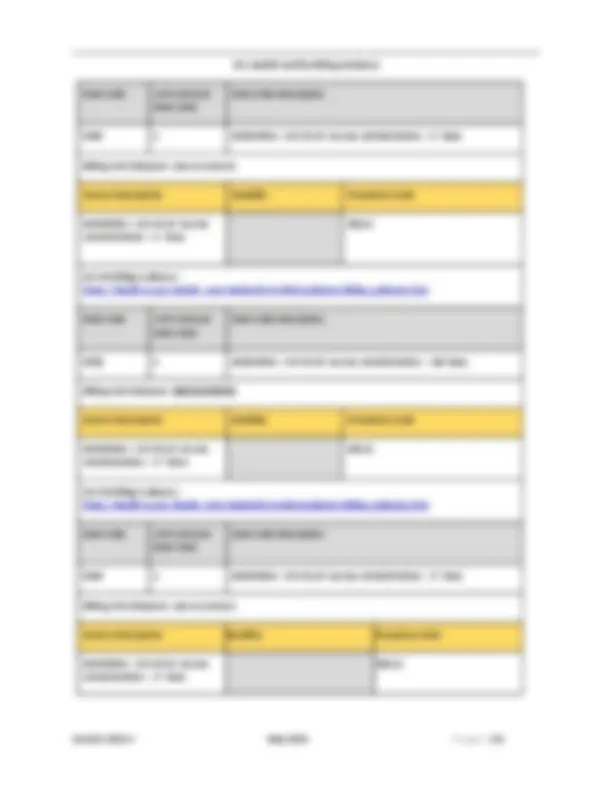
4.9 SUBMITTING OTHER LIMITED HEALTH-RELATED SERVICES CLAIMS FOR DAILY BILLED SERVICES
Other Limited Health-Related Services are billed daily. When submitting an MMCP claim for Other Limited Health-Related Services delivered to the same child/youth on the same date and under the same rate code, submit one claim for each rate code. On each claim, report the procedure codes that reflect the services delivered during the encounter that are applicable to the rate code. If the procedure codes are billable, the units should reflect the length of the encounter related to each billable procedure code. Non-billable procedure codes will have zero units and will not be reimbursed; however, they should be reported on the claim to accurately represent services delivered during the encounter. Each rate code should be billed on separate claim.
When an MMCP has a contract with a Behavioral Health Organization (BHO) to assist with review and processing of behavioral health claims, it may result in the need for providers to send behavioral health claims directly to the BHO and physical health claims to the MMCP. Providers must be aware of these agreements and be able to route claims to the appropriate place for timely reimbursement. The provider should speak directly to the MMCP they have contracted with for additional information.
4.10 OTHER LIMITED HEALTH-RELATED SERVICES CODING TABLE
Appendix C lists the common rate codes, CPT codes, and modifier code combinations that will be required to bill Medicaid Managed Care for the Other Limited Health-Related Services.
Providers can add additional CPT codes, if appropriate, with the rate code descriptions outlined in this manual and consistent with CPT coding standards.
Laboratory services must be billed using the Laboratory Fee schedule found at https://www.emedny.org/ProviderManuals/Laboratory/index.aspx.
CFTSS and HCBS codes are located in the New York State Children’s Health and Behavioral Health Services Billing and Coding Manual, located at https://www.health.ny.gov/health_care/medicaid/redesign/behavioral_health/children/docs/b illing_manual.pdf, and any subsequent updates.
4.11 CLAIMS TESTING
To facilitate a smooth transition to Medicaid Managed Care billing, the MMCPs will offer billing/claim submission training to newly contracted providers and providers in active contract negotiations. This will include testing claims submission and processing, and issuance of MMCP contact and support information to assist programs in claim submission.
Providers are expected to test the claims submission process with MMCPs for all delivered services prior to the service implementation date and upon executing a new contract. Claims testing should begin 90 days prior to the implementation date.
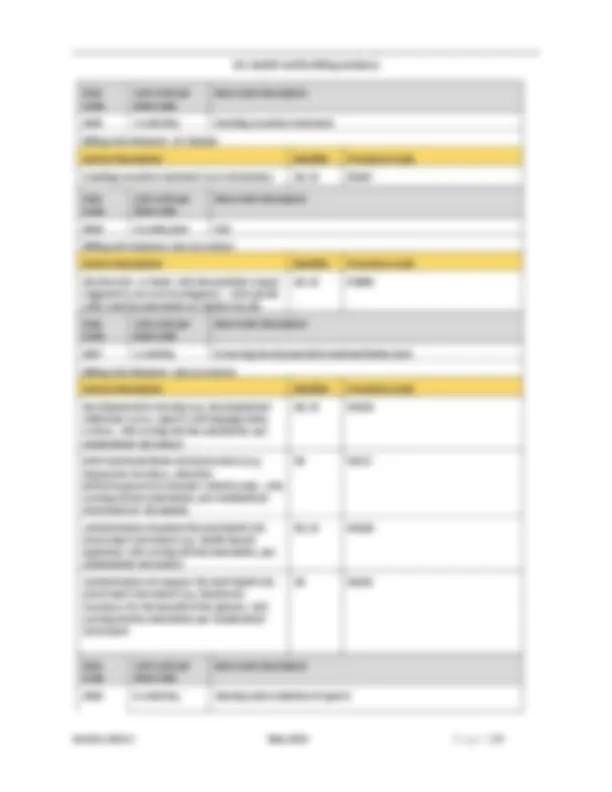
4.12 ABSENCES AND IMPACT ON CLAIMING
The Medicaid residual per diem rate may not be claimed by the 29-I Health Facility when a foster care youth is temporarily absent from the 29-I Health Facility under any circumstances other than those specified in this Manual and future Department updates.
Absence Categories when it is Permissible to Claim the Medicaid Residual Per Diem: It is permissible to claim the Medicaid residual per diem rate for consecutive days one through seven, per episode of absence for the following absence categories: